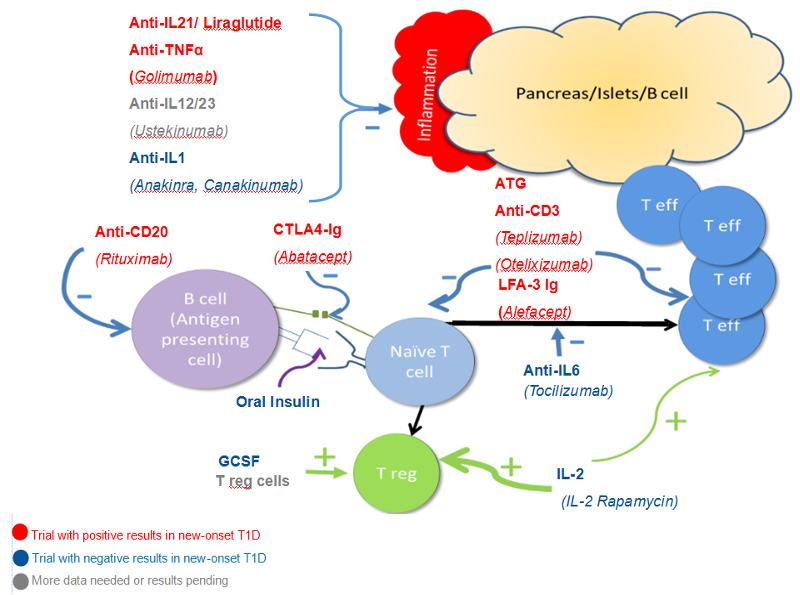
Figure 8. Major pathways leading to beta cell destruction and potential mechanisms underlying the use of selected therapies. Both CD4 and CD8 T effector cells infiltrate and impair/destroy beta cells along with inflammatory cytokines such as IL 21, IL-1 and IL12/23. Anti-IL21/Liraglutide, Golimumab, Ustekinumab, Anakinra, and Canakinumab are aimed at blocking these inflammatory pathways. Activation of Teff cells depends upon presentation of antigen to naïve T cells which result in both Teff turning the immune response “on” and Treg cells turning the immune response “off”. Rituximab decreases B cells and therefore decreases the presentation of antigen to the immune system. Abatacept blocks co-stimulation and oral insulin (and other antigen therapy including the use of antigen specific dendritic cells) alters the response to self-antigen. The aim in both cases is to deviate the response to Treg cells or keep Teff cells from fully activating. ATG and anti-CD3 agents modulate and/or deplete activated T cells. Alefacept has a similar mechanism although primarily aimed at memory T cells. By blocking IL-6, Tocilizumab should change the balance of immune activation towards T regulatory cells. Similarly, GSCF, IL-2 (at the “right dose”), and infusion of Treg cells should preferentially increase Treg cells.
