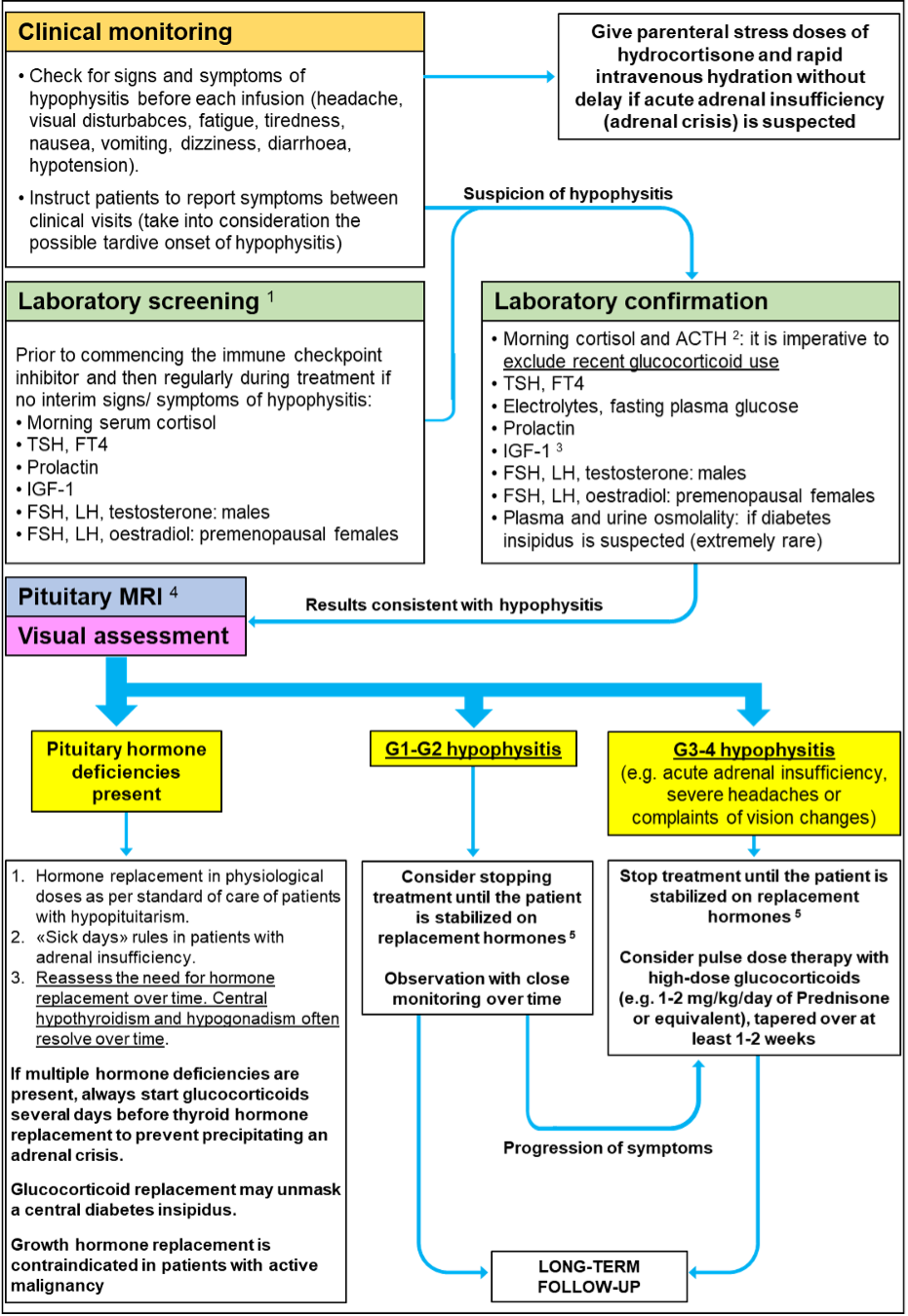
Figure 6. Diagnosis and Management of Immune Checkpoint Inhibitor-Induced Hypophysitis. 1 Some authors suggest laboratory evaluation before the first infusion, then at 8 weeks for patients receiving Ipilimumab (i.e., prior to cycle 3) and then at week 16 if there are no interim signs/symptoms suggestive of hypophysitis. Other authors recommend laboratory evaluation for hypophysitis prior to each infusion of immune checkpoint inhibitors in the first 12-16 weeks of treatment, in order to pick up early or late onset of the disease. 2 Check random ACTH and cortisol if acute adrenal insufficiency is suspected. Exclude recent glucocorticoid use and concomitant treatment that may alter serum cortisol measurement (e.g., oral estrogens). As a guide, in patients that are unwell serum cortisol >450 nmol/L makes the diagnosis of adrenal insufficiency unlikely. Adrenal insufficiency is possible if morning cortisol 200-450 nmol/L or random cortisol 100-450 nmol/L; consider confirmatory testing with Synacthen, although this can give false-positive results in the early stages of central adrenal insufficiency. Adrenal insufficiency is likely if morning cortisol <200 nmol/L or random cortisol <100 nmol/L and patients should be started on hormone replacement. These cut-offs should be seen only as a guide and need to be adapted to local laboratory assays and reference ranges. Patients receiving immune checkpoint inhibitors can also develop adrenalitis and primary adrenal insufficiency. These patients have high ACTH and renin/aldosterone should be measured to investigate mineralocorticoid deficiency. 3 IGF-1 is valuable to confirm changes from baseline that may suggest new-onset hypophysitis. However, further tests to prove GH deficiency are not required because these patients would not be treated (active malignancy). 4 Pituitary MRI is normal in ~20% and ~80% of hypophysitis cases associated with anti-CTLA-4 and anti-PD1/PD1-L1 antibodies, respectively. Therefore, normal imaging does not exclude hypophysitis. MRI changes can be very subtle (Table 11). 5 We believe that patients with immune checkpoint inhibitor-induced hypophysitis should not stop treatment unless they develop severe and progressive symptoms (G3-G4 hypophysitis). Once the acute symptoms of hypophysitis have resolved, restarting treatment with immune checkpoint inhibitors is not contraindicated. Adequately treated, long-term hypopituitarism is not a contraindication to restarting immune checkpoint inhibitors.
