ABSTRACT
Endocrine disorders and the administration of various hormones can alter lipid metabolism and plasma lipid levels, which may increase or decrease the risk of atherosclerotic cardiovascular disease. In many instances the literature is not consistent with various studies reporting different results. These differences may be due to a variety of factors such as the differences in the severity of the disease state, differences in the duration of the disease, underlying genetic factors that differ between individuals and populations, differences in environmental factors such as diet, the presence of other abnormalities that can alter lipid metabolism such as obesity or diabetes, and other unrecognized factors that could influence the expression and manifestation of various endocrine disorders on lipid parameters. Prolactinomas are associated with an increase in total and LDL-C levels. GH deficient patients often have an increase in total cholesterol, LDL-C, and triglyceride levels and a decrease in HDL-C levels, whereas GH therapy decreases total cholesterol and LDL-C but increases Lp(a) levels. Acromegaly is associated with an increase in Lp(a) levels as seen in GH therapy, but paradoxically similar to GH deficiency, acromegaly is accompanied by an increase in plasma triglycerides and a decrease in HDL-C levels. Hypothyroidism leads to an increase in total cholesterol, LDL-C, and Lp(a) levels and normal or increased triglycerides and HDL-C. In contrast, hyperthyroidism is characterized by decreases in total cholesterol, LDL-C, and Lp(a) levels, as well as HDL-C levels. Patients with endogenous Cushing’s syndrome typically display an increase in total cholesterol and LDL-C, and triglycerides, while the administration of glucocorticoids frequently also increases HDL-C levels. Men with low testosterone levels may have high LDL-C and triglyceride levels and decreased HDL-C levels, although this relationship is confounded by obesity and the metabolic syndrome, a common cause of male hypogonadism. Androgen deprivation therapy results in an increase in LDL-C, triglycerides, and Lp(a) and a decrease in HDL-C. The effect of testosterone replacement therapy on plasma lipids and lipoproteins is modest and variable but high dose androgen therapy used by athletes can markedly decrease HDL-C and also reduce Lp(a) levels. The loss of estrogens (postmenopausal females) is associated with a modest increase in LDL-C with either no change or a small decrease in HDL-C. Estrogen administration decreases LDL-C and Lp(a) levels while increasing triglycerides and HDL-C levels but these effects are dependent on the dose and route of administration (transdermal has smaller effects than oral). Concurrent progesterone treatment has little or no effect on the decrease in LDL-C induced by estrogen administration but may blunt the estrogen effect on HDL-C and triglyceride levels depending on the androgenicity of the progesterone. The polycystic ovarian syndrome is associated with increases in LDL-C, triglycerides, and Lp(a) and decreases in HDL-C. The dyslipidemia that occurs with prolactinomas, GH deficiency, hypothyroidism, Cushing’s syndrome, male hypogonadism, androgen deprivation therapy, polycystic ovarian syndrome, and the loss of estrogens may contribute to an increased risk of atherosclerotic cardiovascular disease.
INTRODUCTION
Endocrine disorders and the administration of various hormones can alter lipid metabolism and plasma lipid levels, which may increase or decrease the risk of atherosclerotic cardiovascular disease (ASCVD). In this chapter we will discuss the effects of a number of endocrine disorders on lipid metabolism and plasma lipid and lipoprotein levels. It is worth noting that in many instances the literature is not consistent with various studies reporting different results. These differences may be due to a variety of factors such as the differences in the severity of the disease state, differences in the duration of the disease, underlying genetic factors that differ between individuals and populations, differences in environmental factors such as diet, the presence of other abnormalities that can alter lipid metabolism such as obesity or diabetes, and other unrecognized factors that could influence the expression and manifestation of various endocrine disorders on lipid parameters. In describing the alterations in lipid metabolism and plasma lipid and lipoprotein levels induced by various endocrine disorders we have tried to describe the typical alterations that have been most consistently observed, recognizing that these changes have not been observed in certain published reports and cannot be extrapolated to individual patients.
PROLACTINOMA
Effect of Prolactinomas on Lipid and Lipoprotein Levels
Most studies have shown that patients with a prolactinoma have modestly elevated plasma total cholesterol and LDL-C levels (1-8). In some studies plasma triglyceride levels are also elevated (1,2,4,8-10). HDL-C levels have been reported to be decreased in some studies (7,8,10,11). Most studies have primarily included female patients with prolactinomas but dyslipidemia is also observed in men with hyperprolactinemia (4).
|
Table 1. Effect of Hyperprolactinemia on Lipid and Lipoprotein Levels |
|
|
Total Cholesterol |
|
|
LDL-C |
Increase |
|
HDL-C |
No Change or Decrease |
|
Triglycerides |
No Change or Increase |
The mechanisms accounting for the alterations in plasma lipid levels are not clear but could be related to a number of factors. First, prolactin may have direct effects on lipid metabolism. For example, prolactin decreases lipoprotein lipase activity in human adipose tissue and plasma lipoprotein lipase activity is decreased in patients with prolactinomas, which could increase triglyceride levels (2,12). Second, elevated prolactin levels are associated with decreased estrogen levels in women, a change that is associated with elevated LDL-C and decreased HDL-C levels. Third, elevated prolactin levels are associated with obesity, which could adversely affect plasma lipid levels (1). Finally, with large prolactinomas the secretion of growth hormone (GH) may be impaired, which can result in abnormal plasma lipid levels (2).
Lowering prolactin levels with dopamine agonists, such as bromocriptine or cabergoline, has been shown to decrease plasma total and LDL-C levels and in some instances triglycerides (1,6-8,13-19). However, it is unclear if this effect is solely due to lowering prolactin levels or to other effects of dopamine agonists. The administration of dopamine agonists to patients without prolactinomas has also been shown to induce changes in plasma lipid levels (20). It should be noted that in patients with very high prolactin levels (1355ug/L) pituitary surgery rapidly lowered prolactin levels (77ug/L) and a statistically significant decrease in total cholesterol and triglyceride levels was seen (21). LDL-C levels were also decreased 8.8% but didn’t achieve statistical significance perhaps due to the small number of patients studied (n=17). This observation suggests that lowering prolactin has beneficial effects on the lipid profile.
Risk of Atherosclerotic Cardiovascular Disease (ASCVD)
In patients with prolactinomas, carotid-intima media thickness has been shown to be increased (9,10,22). Moreover, a positive association of serum prolactin concentrations with all-cause and cardiovascular mortality and events has been reported (23,24). This increase in cardiovascular mortality has been particularly noted in males with elevated prolactin levels (25,26). These results suggest that hyperprolactinemia might increase the risk of ASCVD. While prolactin induced abnormalities in lipids could contribute to this increased risk, it should be recognized that elevated prolactin levels also induce other metabolic abnormalities such as obesity, pro-inflammatory state, insulin resistance, and alterations in glucose metabolism that could accelerate atherosclerosis (8).
GROWTH HORMONE DEFICIENCY
Effect of Growth Hormone Deficiency on Lipid and Lipoprotein Levels
Dyslipidemia is commonly observed in adults with growth hormone (GH) deficiency (27-34). Plasma total cholesterol, LDL-C, and triglyceride levels are elevated while HDL-C levels are decreased. Some studies reporting no difference in LDL size and others an increase in small dense LDL while Lp(a) levels in controls and in GH deficient patients are similar (30,31,35,36). It should be recognized that GH deficiency leads to increased adiposity, which may be an important contributor to dyslipidemia (37). However, even when controlling for BMI, dyslipidemia is still present in GH deficient patients (27).
|
Table 2. Effect of Growth Hormone Deficiency on Lipid and Lipoprotein Levels
|
|
|
Total Cholesterol |
Increase |
|
LDL-C |
Increase |
|
HDL-C |
Decrease |
|
Triglycerides |
Increase |
|
Lp (a) |
No change |
Effect of Growth Hormone Therapy on Lipid and Lipoprotein Levels
Numerous studies have examined the effect of GH replacement therapy on serum lipid levels. A meta-analysis by Newman and colleagues reported on the effect of low dose GH replacement (<0.7mg/day; seven studies) and high dose GH replacement (>0.7mg/day; sixteen studies) involving over 1000 subjects (38). In both the low dose and high dose groups, GH replacement therapy decreased total and LDL-C levels but did not significantly affect either HDL-C or triglyceride levels. LDL-C levels were decreased by 11.3%. A meta-analysis of 37 trials by Maison et al also found that total and LDL-C levels were decreased with no significant changes in triglycerides or HDL-C by GH treatment (39). In a few studies, HDL-C levels have been observed to increase with GH therapy (32,40,41). For example, in a 15 year long term perspective study GH therapy reduced LDL-C and increased HDL-C levels, while having no significant effect on triglyceride levels (42). The ability of GH therapy to decrease LDL-C levels occurs even when patients are on statin therapy (43). Moreover, the decrease in LDL-C levels with GH treatment correlates with baseline LDL-C levels (i.e. the higher the LDL-C the greater the decrease with GH treatment) (44). Interestingly GH treatment increases Lp(a) levels (41,45-52). Of note, studies have shown that treatment with GH increases Lp(a) levels while treatment with IGF-1 decreases Lp(a) levels (53). Whether this increase in Lp(a) levels will enhance the risk of cardiovascular disease is unknown.
|
Table 3. Effect of Growth Hormone Therapy on Lipid and Lipoprotein Levels |
|
|
Total Cholesterol |
Decrease |
|
LDL-C |
Decrease |
|
HDL-C |
No Change or Increase |
|
Triglycerides |
No Change |
|
Lp (a) |
Increase |
Mechanism for the Changes in Lipids and Lipoproteins in GH Deficiency
LDL-C
Studies have shown that GH increases the expression of hepatic LDL receptors (54,55). Additionally, GH decreases circulating PCSK9 levels, which would also increase hepatic LDL receptors (56). As a consequence, the clearance of LDL-C is accelerated by GH treatment (57,58). Thus, the increase in total cholesterol and LDL-C levels in GH deficient patients is likely due to a decrease in hepatic LDL receptors and therefore with GH administration the number of LDL receptors increases leading to a decrease in plasma LDL-C levels. Notably, in a patient with homozygous familial hypercholesterolemia, devoid of functional LDL receptors, GH treatment did not result in a decrease in LDL-C levels, whereas in GH deficient patients, normal subjects, and patients with heterozygous familial hypercholesterolemia treatment with GH resulted in a decrease in LDL-C levels (57). This observation further demonstrates the importance of LDL receptors in mediating the decrease in LDL-C levels in response to GH administration.
TRIGLYCERIDES
In GH deficient patients there is an increase in hepatic VLDL production and a reduction in VLDL clearance, which together could lead to an increase in plasma triglyceride levels (59). GH therapy stimulates VLDL secretion and increases VLDL clearance, which is likely due to its effects in up-regulating low density lipoprotein receptors, leading to a neutral effect on plasma triglyceride levels (60). The enhancement in VLDL secretion by GH treatment is likely facilitated by the well-recognized ability of GH to stimulate lipolysis in adipose tissue, which will provide fatty acids for the synthesis of triglycerides in the liver and enhance VLDL production (61). GH increases fatty acid oxidation but this may not be able to offset the increased lipolysis and VLDL production (62).
LIPOPROTEIN (a)
In transgenic mice expressing the human Apo (a) gene, GH administration increases the mRNA levels of Apo (a) and plasma levels of Apo (a) (63). The increased production of Apo (a) induced by GH could account for the increase in Lp(a) levels induced by GH treatment.
Risk of Cardiovascular Disease
Several observational studies have found that patients with hypopituitarism on conventional replacement therapy have an increased mortality that is primarily due to cardiovascular and cerebrovascular disease (64-68). Additionally, the risk of myocardial infarctions is increased in hypopituitarism (64,69). Moreover, increased coronary artery calcifications and carotid intima-media thickness have been observed in patients with GH deficiency (33,70-77). It is likely that the dyslipidemia that commonly occurs in GH deficient patients contributes to this increased risk of cardiovascular disease. However, GH deficient patients also display an increase in visceral adiposity, insulin resistance, impaired glucose metabolism, an increased prevalence of the metabolic syndrome, and an increased pro-inflammatory state with elevations in C-reactive protein and inflammatory cytokines, which could also contribute to an increased risk of cardiovascular disease (40). Since GH deficient patients have an increased risk of ASCVD one could consider GH deficiency as a risk enhancer when evaluating patients for lipid lowering therapy.
Whether treating GH deficient patients with GH replacement therapy reduces the risk of cardiovascular disease is uncertain, as there are no long-term randomized outcome studies. There are however a number of observational studies. Svensson and colleagues reported that in patients with hypopituitarism on GH replacement therapy the risk of myocardial infarctions was decreased but the occurrence of cerebrovascular events appeared to be increased compared to untreated patients (64). Bengtsson and colleagues reported that morbidity was not increased in patients with GH deficiency who were treated with GH compared to the general population and was even reduced compared to untreated patients (78). Holmer et al reported that in GH deficient patients, the risk of nonfatal stroke declined in males and females and nonfatal cardiac events decreased in males treated with GH replacement therapy (79). Finally, van Bunderen et al reported that GH deficient men receiving GH treatment had a mortality rate similar to the background population but women had an increase in cardiovascular mortality (80). Together these results suggest that GH therapy may reduce the risk of cardiovascular disease.
In non-randomized trials a decrease in carotid intima-media thickness was observed in GH deficient patients treated with GH (71,74,75,77,81-83). Other similar studies have not shown a decrease in carotid intima-media thickness with GH treatment [61]. Furthermore, in Brazilian patients with lifelong isolated GH deficiency, treatment with GH increased carotid intima-media thickness (84).
Thus, at this time it is uncertain whether GH replacement therapy will have beneficial effects on long term ASCVD outcomes. Randomized outcome trials will be required to definitively answer this question.
ACROMEGALY
Effect of Acromegaly on Lipid and Lipoprotein Levels
In patients with acromegaly an increase in plasma triglyceride levels and a decrease in HDL-C levels have been frequently observed (85-95). In one large retrospective study of 307 newly diagnosed patients with acromegaly, 33% of patients were noted to have elevated triglyceride levels (>150mg/dl) while 17% of men and 62% of women had low HDL-C levels defined by metabolic syndrome criteria (96). The effect of acromegaly on total cholesterol and LDL-C levels has been variable (85,86,88-91,93-95,97-100). However, an increase in small dense LDL levels and Apo B levels may be seen (92-94,101). Additionally, an increase in Lp(a) levels has been reported in several studies (94,99,102-104).
|
Table 4. Effect of Acromegaly on Lipid and Lipoprotein Levels
|
|
|
Total Cholesterol |
Variable |
|
LDL-C |
Variable |
|
HDL-C |
Decrease |
|
Triglycerides |
Increase |
|
Lp (a) |
Increase |
Treatment of acromegaly that normalizes GH and IGF-1 levels typically results in a decrease in plasma triglyceride levels and an increase in HDL-C levels (89,90,94,104-111). Additionally, small dense LDL and Lp(a) levels may also decrease (94,97,102-104,106-108). Interestingly, the GH-receptor antagonist, pegvisomant, increased TG levels in healthy men (112) and increased total and LDL-C levels and decreased Lp(a) levels in patients with acromegaly (97,98).
Mechanism for the Changes in Lipids and Lipoproteins in Acromegaly
TRIGLYCERIDES
The increase in plasma triglycerides has been shown to be associated with an increased triglyceride production rate (87). Treatment with GH stimulates VLDL secretion, which is likely facilitated by the ability of GH to enhance lipolysis that will provide fatty acids for the synthesis of triglycerides in the liver, thereby enhancing VLDL production (60,61). In addition, several studies have shown that lipoprotein lipase activity is decreased in patients with acromegaly, which could decrease the clearance of triglyceride rich lipoproteins (86,113,114). It is likely that the insulin resistance and abnormal glucose metabolism that frequently occurs in patients with acromegaly also contributes to the abnormalities in triglyceride metabolism.
HDL-C
LCAT, hepatic lipase, and phospholipid transfer protein have all been reported to be decreased in patients with acromegaly while some studies have shown a decrease in CETP and others an increase (93,95,101). Whether these changes account for the decrease in HDL-C levels is uncertain. A decrease in LCAT, CETP, and hepatic lipase could result in a decrease in reverse cholesterol transport (115).
LIPOPROTEIN (a)
In transgenic mice expressing the human Apo (a) gene, GH administration increases the mRNA levels of Apo (a) and plasma levels of Apo (a) (63). The increased production of Apo (a) induced by GH could account for the increase in Lp(a) levels in patients with acromegaly. Of note studies have shown that treatment with GH increases Lp(a) levels however treatment with IGF-1 decreases Lp(a) levels (53).
Risk of Cardiovascular Disease
Cardiovascular disease is increased in patients with acromegaly but much of this is related to acromegalic cardiomyopathy, valvular heart disease, and arrhythmias (116,117). It remains uncertain whether atherosclerotic cardiovascular disease is increased (116,117). A study using the German Acromegaly Registry did not observe an increase in myocardial infarctions or strokes in 479 patients with acromegaly compared to the general population (118). Similarly, a large cohort study from Korea with over 1800 patients with acromegaly also did not observe an increase in atherosclerotic cardiovascular disease events (119). Several studies have shown an increase in carotid intima-media thickness in patients with acromegaly (89,90,120-124). However, a study by Otsuki and colleagues showed that if one controls for risk factors carotid intima-media thickness in patients with acromegaly was similar to matched controls (125). In contrast, Ozkan and colleagues found that carotid intima-media thickness in patients with acromegaly was still increased even in matched controls (124). Several studies have shown that the treatment of acromegaly results in a decrease in carotid intima-media thickness (89,90,122,126). In contrast to the results seen in studies of carotid intima-media thickness, studies of coronary artery calcium score in patients with acromegaly have not consistently shown an increase in atherosclerosis. While Cannavo et al have shown an increase in coronary artery calcium, other studies have not shown an increase (127-130). In the study of Herrmann et al the coronary artery calcium score directly correlated with disease duration suggesting that patients with long standing acromegaly are more likely to develop atherosclerosis (131). Thus, whether acromegaly increases atherosclerosis and atherosclerotic cardiovascular disease events requires further investigation.
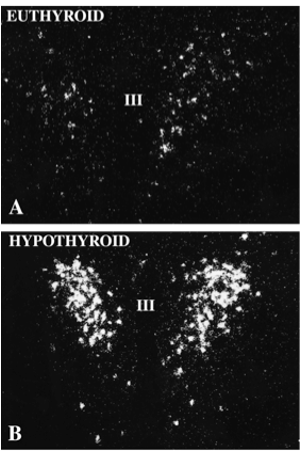
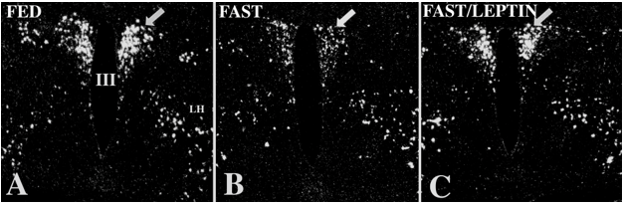
HYPOTHYROIDISM
Effect of Hypothyroidism on Lipid and Lipoprotein Levels
It has been recognized since the 1930s that hypothyroidism results in an increase in plasma cholesterol levels (132). Indeed, along with protein bound iodine, cholesterol levels were followed as a marker for treatment before immunoassays were developed for TSH and FT4. The lipid profile of hypothyroid patients is characterized by an increase in total and LDL-C levels (132). LDL-C levels can be strikingly elevated, sometimes raising the suspicion of familial hypercholesterolemia. Hypothyroidism can also unmask familial dysbetalipoproteinemia (Type III hyperlipidemia) (133-135). In most studies there is not an increase in small dense LDL (132). It should be routine clinical practice to determine thyroid function in patients with significant elevations in LDL-C to rule out hypothyroidism as the cause of the hypercholesterolemia. The effect of hypothyroidism on HDL-C levels is variable with either no change or a modest increase in HDL-C levels but there is a more consistent increase in the concentration of HDL 2 particles (132,136). Similarly, hypothyroidism has either no effect or modestly increases plasma triglyceride levels (132). Of note, Lp(a) levels are also increased in hypothyroid patients (132,137-141). In a study of 295 patients with overt hypothyroidism 56% had elevations in LDL-C, 34% had elevated LDL-C and elevated triglyceride levels, 1.5% had elevations only in triglycerides, and 8.5% had no lipid abnormalities (142). Patients with secondary hypothyroidism were more likely to have elevations in both LDL-C and triglyceride levels in this study (142). However, other studies have not observed a difference in the dyslipidemia in patients with primary or secondary hypothyroidism (143). In general, the changes in lipids and lipoprotein induced by hypothyroidism are pro-atherogenic and are more severe with severe hypothyroidism. Restoration of thyroid function improves the lipid abnormalities towards normal (132,142,144,145). A meta-analysis by Kotwal et al demonstrated that the treatment of hypothyroidism with levothyroxine resulted in a decrease in total cholesterol by -58 mg/dL (95% CI: -64.7, -52.1), LDL-C by -41 mg/dL (95% CI: -46.5, -35.7), HDL-C by -4.1 mg/dL (95% CI: -5.67, -2.61), triglycerides by -7.3 mg/dL (95% CI: -36.63, 17.87), apo A by -12.6 mg/dL (95% CI: -17.98, -7.19), apo B by -34.0 mg/dL (95% CI: 41.14, -26.77), and Lp(a) by -5.6 mg/dL (95% CI: -9.06, -2.14) (146).
|
Table 5. Effect of Hypothyroidism on Lipid and Lipoprotein Levels
|
||
|
|
Overt Hypothyroidism |
Subclinical Hypothyroidism |
|
Total Cholesterol |
Increase |
Normal to increased |
|
LDL-C |
Increase |
Normal to increased |
|
HDL-C |
Normal to slightly increased |
No change |
|
Triglycerides |
Normal to increase |
Normal to increased |
|
Lp(a) |
Increase |
No change |
|
Apo B |
Increase |
Increase |
|
Apo A-I |
Increase |
No change |
Subclinical Hypothyroidism
The effects of subclinical hypothyroidism on lipid and lipoprotein levels have been highly variable with some studies showing changes similar to what is observed in patients with overt hypothyroidism and other studies showing no differences in patients with subclinical hypothyroidism compared to controls (147,148). These differences are likely related the types of patients included in the studies with variables such as age, ethnicity, duration of hypothyroid dysfunction, and the presence of other metabolic abnormalities such as insulin resistance (149). One key variable is the degree of thyroid dysfunction with studies that included patients with higher TSH levels (>10mIU/L) more likely to show that subclinical hypothyroidism is associated with abnormalities in lipid and lipoprotein levels (148).
An important issue in patients with subclinical hypothyroidism is whether one should treat with thyroid hormone replacement or just observe. Because of this uncertainty it has been of great interest to determine if the lipid profile in patients with subclinical hypothyroidism improves with thyroid hormone treatment. A large number of studies have explored this issue but the results have likewise been inconsistent with some studies showing potentially beneficial changes in the lipid profile and other studies showing no changes with treatment of subclinical hypothyroidism (147,148). A recent review also did not find firm evidence of a beneficial effect on the lipid profile with thyroid hormone treatment in patients with subclinical hypothyroidism (150). A meta-analysis by Kotwal et al demonstrated that the treatment of subclinical hypothyroidism with levothyroxine resulted in a decrease in total cholesterol by -12 mg/dL, LDL-C by -11 mg/dL, triglycerides by -4.5 mg/dL, apo B by -6.6 mg/dL, and Lp(a) by -1.99 mg/dL with no significant changes in HDL-C or apo AI (146). However, when this meta-analysis only included studies with either a placebo or observational control group they did not demonstrate any significant changes in lipids with levothyroxine therapy (146). It is likely that the patients with higher TSH levels and higher LDL-C levels will benefit from treatment with L-thyroxine (151).
Risk of Cardiovascular Disease in Subclinical Hypothyroidism
A major issue in patients with subclinical hypothyroidism is whether they are at increased risk of developing cardiovascular disease. Some but not all meta-analyses have suggested that subclinical hypothyroidism is associated with a small increase in cardiovascular risk particularly in young patients and patients whose TSH is greater than 10mIU/L (147,152-156). The length of time that a patient is hypothyroid and the degree of elevation of cholesterol may be important factors. Whether thyroid treatment lowers this risk is uncertain with some observational studies reporting a benefit and others reporting no benefit (147,148,157). No randomized outcome studies have addressed whether treatment with thyroid hormone will reduce cardiovascular events in patients with subclinical hypothyroidism and without such studies it is difficult to be certain whether thyroid hormone replacement is indicated.
In patients with subclinical hypothyroidism carotid intima-media thickness (cIMT) is increased and two meta-analyses found that thyroid hormone treatment reduced cIMT suggesting a possible beneficial effect on atherosclerosis (158-160). This decrease in cIMT was associated with a reduction in plasma lipid levels. However, it should be noted that a recent randomized study of 185 subjects with subclinical hypothyroidism (TSH 6.35mIU/L) did not find any difference in cIMT after 18 months in the thyroid hormone treated group compared to the placebo group (161). Only a small number of studies have examined coronary calcium scores but the limited data suggest an increase in coronary calcium in individuals with subclinical hypothyroidism (162-165).
It is recommended by the American Thyroid Association, and the American Association of Clinical Endocrinologists that subclinical hypothyroidism should be treated when the TSH level is >10 mIU/L (157). Routine treatment for patients with TSH levels between 4.5 and 10mIU/L is not recommended but one can decide to initiate therapy based on individual factors, such as antibodies and symptoms (157). There are no recommendations by these societies to treat with thyroid hormone replacement for the purpose of correcting abnormal lipid and lipoprotein levels or reducing cardiovascular risk. Since randomized clinical trials have not consistently shown a lipid-lowering benefit with thyroid hormone therapy in patients with subclinical hypothyroidism (TSH < 10mIU/L), patients with significant hyperlipidemia, should be treated with lifestyle changes and lipid-lowering medications.
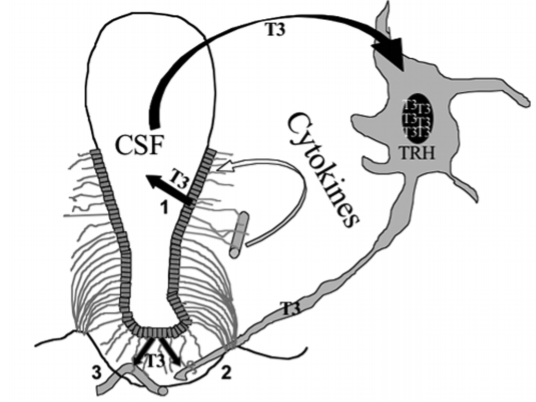
Mechanism for the Changes in Lipids and Lipoproteins in Hypothyroidism
Thyroid hormone regulates the expression and activity of a number of key enzymes and receptors that regulate lipid and lipoprotein levels.
LDL-C
The primary mechanism by which hypothyroidism results in elevated total cholesterol and LDL-C levels is via a decrease in LDL receptor levels in the liver. Thyroid hormone stimulates the expression of LDL receptors and in hypothyroidism the number of hepatic LDL receptors is reduced leading to the decreased clearance of circulating LDL (132,166-171). This decreased clearance of LDL accounts for the increase in plasma LDL levels. Thyroid hormone stimulates LDL receptor expression by increasing SREBP-2 and/or by direct effects on the LDL receptor promoter (172,173). Finally, PCSK9 levels are increased with hypothyroidism, which could further contribute to a decrease in hepatic LDL receptor levels by accelerating the catabolism of LDL receptors (174,175). Interestingly, treatment of HepG2 cells in vitro with TSH stimulated PCSK9 expression and decreased LDL receptors (175)
In addition to the effects on the LDL receptor levels, other changes induced by thyroid hormone may also contribute to the increases in LDL-C levels in hypothyroid patients. Studies in LDL receptor deficient mice (LDL receptor knock-out mice) have shown that thyroid hormone administration lowers LDL-C levels despite the absence of LDL receptors(176,177).Thyroid hormone also stimulates the conversion of cholesterol to bile acids by increasing cholesterol 7 alpha hydroxylase, the initial enzyme in bile acid synthesis, and in hypothyroid patients a decrease in bile acid synthesis could contribute to an increase in LDL-C levels (174,177-180). Furthermore, the expression of ABCG5 and ABCG8, the transporters that mediate the movement of cholesterol from the hepatocyte into the bile, are also stimulated by thyroid hormone (181,182). In addition, studies by Goldberg and colleagues demonstrated that thyroid hormone decreases Apo B production and hence in hypothyroidism there could be an increase in Apo B synthesis (176). Finally, studies have shown that hypothyroidism is associated with increased intestinal cholesterol absorption that is due to an increase in NPC1L1 (181). Thus, a number of potential pathways could contribute to the increased LDL-C that occurs in hypothyroidism.
TRIGLYCERIDES
As noted above hypothyroidism has only modest effects on plasma triglyceride levels. Several but not all studies have shown that thyroid hormone stimulates lipoprotein lipase activity (183-188). A decrease in lipoprotein lipase activity could lead to the decreased clearance of triglyceride rich lipoproteins accounting for the increase in plasma triglyceride levels in hypothyroidism. Moreover, studies have shown that thyroid hormone stimulates the expression of Apo A-V, which potentiates the activity of lipoprotein lipase, and is associated with decreases in plasma triglyceride levels (189). Additionally, thyroid hormone decreases angiopoietin-like proteins 3 and 8, inhibitors of lipoprotein lipase, and the levels of angiopoietin-like proteins 3 and 8 are elevated in hypothyroid patients which could lead to a decrease in lipoprotein lipase activity (190,191). Lastly, hypothyroidism increases hepatic VLDL-TG secretion rate, which could also contribute to elevations in plasma triglyceride levels (192).
HDL-C
As noted above hypothyroidism has only modest effects on plasma HDL-C levels. However, thyroid hormone might be having effects on HDL metabolism that are not reflected in HDL-C levels, as a number of key proteins involved in HDL metabolism and reverse cholesterol transport are regulated by thyroid hormone. Specifically, CETP, hepatic lipase, LCAT, and SR-B1 are increased by thyroid hormone and are decreased in hypothyroidism (182,183,185,188,193-200). A decrease in CETP, hepatic lipase, LCAT, and SR-B1 would be anticipated to result in a decrease in reverse cholesterol transport (115). Moreover, sera from animals treated with thyroid hormone have the increased ability to facilitate the efflux of cholesterol from macrophages to HDL via ABCA1 (201).
LIPOPROTEIN (a)
The mechanism for the increase in Lp(a) is unknown.
HYPERTHYROIDISM
Effect of Hyperthyroidism on Lipid and Lipoprotein Levels
In hyperthyroidism total cholesterol and LDL-C levels are decreased (132,202). Additionally, HDL-C and Lp(a) levels are also decreased (132,202) (Table 6). The effect on triglyceride levels is variable and triglyceride levels may be increased, decreased, or unchanged (132,202). Restoration of euthyroidism results in the normalization of lipid and lipoprotein levels. A meta-analysis reported that treatment of hyperthyroidism resulted in a significant increase in total cholesterol (44.5mg/dL; 95% CI: 38.0 - 51.0), LDL-C (31.1mg/dL; 95% CI 24.3- 37.9), HDL-C (5.52mg/dL; 95% CI 1.48- 9.56), Apo AI (15.6 mg/dL; 95% CI; 10.4- 20.8), apo B (26.1mg/dL; 95% CI 22.7- 29.6), and Lp[a] (4.18mg/dL; 95% CI; 1.65- 6.71) with no significant change in triglyceride levels (146). Treatment of subclinical hyperthyroidism did not change any lipid parameters significantly (146). A recent small study reported that patients with severe subclinical hyperthyroidism (TSH <0.1 mlU/L) treated with radioactive iodine had increases in total cholesterol (16.7 ± 4.5mg/dL; p < 0.01), LDL-C (14.3 ± 4.1mg/dL; p < 0.01) and triglycerides (25.2±9.4mg/dL; p< 0.01) while patients with mild subclinical hyperthyroidism (TSH: 0.1-0.39 mlU/L) did not demonstrate statistically significant increases in lipid levels (203).
|
Table 6. Effect of Hyperthyroidism on Lipid and Lipoprotein Levels
|
|
|
Total Cholesterol |
Decrease |
|
LDL-C |
Decrease |
|
HDL-C |
Decrease |
|
Triglycerides |
Variable |
|
Lp(a) |
Decrease |
|
Apo B |
Decrease |
|
Apo A-I |
Decrease |
Given the beneficial effects of thyroid hormone on lipid and lipoprotein levels, consideration has been given to treating patients with thyroid hormone/thyroid hormone analogues to reduce cardiovascular disease. The Coronary Drug Project examined the use of D-thyroxine for lipid lowering in patients with cardiovascular disease. While D-thyroxine was effective in lowering LDL-C levels, it was also associated with an increase in cardiovascular deaths and the trial was therefore stopped early (204). More recently there have been efforts by the pharmaceutical industry to develop thyroid hormone analogs and mimetics that would have the beneficial effects of thyroid hormone on lipids and lipoproteins without inducing the harmful effects of excess thyroid hormone (205).
Mechanism for the Changes in Lipids and Lipoproteins in Hyperthyroidism
Thyroid hormone regulates the expression and activity of a number of key enzymes and receptors that regulate lipid and lipoprotein levels. For details see section on hypothyroidism.
LDL-C
The decrease in LDL-C levels is primarily due to an increase in hepatic LDL receptors resulting in the accelerated clearance of circulating LDL (132). This increase in LDL receptors is due to thyroid hormone stimulating the increased expression of LDL receptors (132,172,173). In addition, hyperthyroidism leads to a decrease in PCSK9, which will lead to a decrease in the degradation in LDL receptors contributing to the increase in LDL receptors (174).
Studies in LDL receptor deficient mice (LDL receptor knock-out mice) have shown that thyroid hormone administration lowers LDL levels despite the absence of LDL receptors, indicating that factors in addition to up-regulation of the LDL could contribute to the decrease in circulating LDL [167, 168]. Thyroid hormone stimulates the elimination of cholesterol from the body by increasing the conversion of cholesterol into bile acids and increasing the biliary secretion of bile acids and cholesterol (174,179,180,206). Thyroid hormone also diminishes intestinal absorption of dietary cholesterol (181). Finally, thyroid hormone decreases Apo B production and hence hyperthyroidism could result in a decrease in Apo B synthesis [167]. The relative contribution of these changes in contributing to the decrease in LDL-C is unknown.
HDL-C
A number of key proteins involved in HDL metabolism and reverse cholesterol transport are regulated by thyroid hormone. Specifically, CETP, hepatic lipase, LCAT, and SR-B1 are increased by thyroid hormone (182,183,185,188,193-200). An increase in CETP, hepatic lipase, LCAT, and SR-B1 would be anticipated to result in a decrease in HDL-C and an increase in reverse cholesterol transport (115). Moreover, sera from animals treated with thyroid hormone have the increased ability to facilitate the efflux of cholesterol from macrophages to HDL via ABCA1 (201).
LIPOPROTEIN (a)
The mechanism for the decrease in Lp(a) is unknown. Studies have shown that decreases in PCSK9 activity can reduce Lp(a) levels so perhaps the thyroid hormone induced decrease in PCSK9 plays a role (174,207).
CUSHING’S SYNDROME
Effect of Cushing’s Syndrome on Lipid and Lipoprotein Levels
It is difficult to state the true prevalence of hyperlipidemia in patients with Cushing’s syndrome due to the fact that cut-offs used to establish the presence of hyperlipidemia vary among different studies and the number of patients in these studies have been relatively small. Additionally, the severity of the Cushing’s syndrome is also a key variable. Nevertheless, it is apparent that dyslipidemia is a common feature of Cushing’s syndrome with an elevation in plasma triglycerides and total cholesterol due to an increase in circulating VLDL and LDL (208-214). The elevation in total and LDL-C levels correlates with the severity of the Cushing’s syndrome (208,210). A comparison of ACTH-dependent and ACTH-independent Cushing syndrome did not observe differences in lipid levels (215). The central obesity that characterizes Cushing’s syndrome likely contributes to the dyslipidemia with patients who have central obesity more likely to have alterations in lipid levels (214). Additionally, if Cushing’s syndrome is associated with diabetes this can further alter lipid and lipoprotein levels (216). These alterations in lipid and lipoprotein levels improve or normalize after treatment and lowering of the elevated cortisol levels (208,217). The effect of Cushing’s syndrome on HDL-C is more variable with increases and decreases in HDL-C both being reported in different studies (208,209). Finally in one small study Lp(a) levels were not altered in patients with Cushing’s syndrome (218), while in another small study Lp(a) levels were increased (214).
Most series report improvement in hyperlipidemia with correction of elevated cortisol levels, though a complete normalization of lipid parameters is frequently not achieved (208). In a longitudinal study, 25 patients had a significant decrease in LDL-C levels after one year of normalization of cortisol levels, but levels still remained higher than healthy controls, albeit similar to BMI-matched controls (213). Similarly, in a cross-sectional study carried out 5 years after cure or control of pituitary Cushing’s disease, levels of total and LDL-C were similar to levels found in BMI-matched controls, but higher than in normal controls (214).
|
Table 7. Effect of Cushing’s Syndrome on Lipid and Lipoprotein Levels |
|
|
Total Cholesterol |
Increase |
|
LDL-C |
Increase |
|
HDL-C |
Variable |
|
Triglycerides |
Increase |
|
Lp (a) |
No change or increase |
|
Apo B |
Increase |
|
Apo A-I |
Variable |
In patients without inflammatory disorders, the administration of glucocorticoids has variable effects on the lipid profile; HDL-C levels are typically increased with the magnitude of change in plasma triglyceride and LDL-C varying among studies (219-221). In patients with inflammatory diseases, the effect of glucocorticoids on lipids is confounded by the marked anti-inflammatory effects of glucocorticoids. Inflammation affects lipid and lipoprotein levels and thus reducing inflammation per se can affect the lipid response to glucocorticoid treatment (222). Similarly, the effect of glucocorticoids on lipids following transplantation or the treatment of other medical conditions is also difficult to interpret due to the simultaneous use of other medications and the response of the underlying medical conditions. Furthermore, the dose and route of administration of the glucocorticoids can be an important variable, as low doses often have minimal effects on triglyceride, LDL-C, and HDL-C levels while high doses tend to increase serum triglyceride, LDL-C, and HDL-C levels.
|
Table 8. Effect of Glucocorticoid Treatment on Lipid and Lipoprotein Levels |
|
|
Total Cholesterol |
Increase |
|
LDL-C |
No Change or Increase |
|
HDL-C |
Increase |
|
Triglycerides |
No Change or Increase |
Mechanism for the Changes in Lipids and Lipoproteins in Cushing’s Syndrome
The mechanisms by which excess glucocorticoids induce changes in lipid and lipoprotein metabolism have not been precisely elucidated and the literature on this topic is often contradictory (223,224). Below we will review some of the potential mechanisms that could account for the observed changes.
LDL-C
A single study in rats has shown that glucocorticoids decrease hepatic LDL receptor expression (225). However, this glucocorticoid effect on LDL receptor expression was not seen by Galman and colleagues (181). Intriguingly, Galman and colleagues reported that ACTH stimulation of the adrenals did decrease the expression of both hepatic LDL receptors and SR-B1 receptors, suggesting that hormones other than glucocorticoids might have effects on liver receptors (226). Whether this plays a role in the increase in plasma LDL-C levels seen in some individuals with Cushing’s syndrome is unknown.
TRIGLYCERIDES
Glucocorticoid administration stimulates hepatic fatty acid synthesis by increasing the activity of acetyl CoA carboxylase and fatty acid synthesis (223,227-230). In addition, glucocorticoids also stimulate the enzymes required for the synthesis of triglyceride in the liver (231-233). The increase in hepatic triglyceride levels leads to the decreased degradation of Apo B and an increase in the formation and secretion of VLDL (223,224,230,234-236). Moreover, in patients with Cushing’s syndrome VLDL production rates are increased, while VLDL clearance is not altered, indicating that hepatic overproduction of VLDL accounts for the increase in serum triglyceride levels (217). This increase in VLDL production could also contribute to the increase in LDL-C levels in patients with Cushing’s syndrome (217).
In addition to glucocorticoids increasing hepatic fatty acid synthesis, in acute experimental models, glucocorticoids also increase adipose tissue lipolysis resulting in an increase in circulating free fatty acid levels (223,224,237-243). Glucocorticoids increase the expression of adipose tissue triglyceride lipase and hormone sensitive lipase, two of the key enzymes that mediate the breakdown of triglycerides into free fatty acids in adipose tissue (238,241,244,245). Furthermore, glucocorticoids also stimulate adipose tissue lipolysis by increasing cAMP levels, which stimulates the activation of protein kinase A (PKA) leading to the phosphorylation of hormone sensitive lipase and perilipin (237,241). However, studies have shown that chronic elevations in glucocorticoids do not increase adipose tissue lipolysis; thus it is not clear whether increased transport of fatty acids from adipose tissue to liver contributes to the chronic increased formation and secretion of VLDL by the liver (224,246,247)
HDL-C
Studies have shown that glucocorticoids increase the synthesis and secretion of Apo A-I by direct effects on the Apo A-I promoter that are mediated via the glucocorticoid receptor (248,249). The increased production of Apo A-I could lead to an increase in HDL-C. Furthermore, glucocorticoids decrease hepatic lipase activity and increase LCAT activity, which could also contribute to an increase in HDL-C levels (250).
Risk of Cardiovascular Disease
Patients with Cushing’s syndrome have a higher mortality rate than age and gender matched controls, which is mainly due to an increased risk of cardiovascular disease (251-254). Notably this increased mortality risk remains even after remission of Cushing’s syndrome, but is reduced compared to persistent disease (254,255). Furthermore, studies have shown that the hazard ratio for myocardial infarctions was 3.7 and for strokes was 2.0 in patients with Cushing’s syndrome (256). Moreover, patients with Cushing’s syndrome have an increase in carotid intima-media thickness, which persists after remission of the disease (213,214,257-259). Additionally, coronary artery calcium, a marker of atherosclerosis, is also increased in patients with Cushing’s syndrome and also persists after disease remission (260,261). Importantly, iatrogenic Cushing’s syndrome also increases the risk for cardiovascular disease (262-265). Thus, it is quite clear that Cushing’s syndrome increases the risk and occurrence of atherosclerotic cardiovascular disease. It is likely that the dyslipidemia that accompanies Cushing’s syndrome contributes to the increase in atherosclerotic cardiovascular disease, but it must be recognized that Cushing’s syndrome also induces other abnormalities that are highly associated with an increased risk of atherosclerotic cardiovascular disease such as central obesity, diabetes, insulin resistance, hypercoagulability, and hypertension (266,267). It is therefore likely that the increase in atherosclerotic cardiovascular disease seen in patients with Cushing’s syndrome is multifactorial.
Because of an increased risk of cardiovascular disease the Endocrine Society recommends that “in adults with persistent endogenous Cushing syndrome, we suggest statin therapy, as adjunct to lifestyle modification, to reduce CV risk irrespective of the CV risk score” with a goal LDL-C < 70mg/dL (268). Additionally, the Endocrine Society recommends “In adults with cured Cushing syndrome, we advise the approach to CV risk assessment and treatment be the same as in the general population” (268).
Effect of Drugs Used to Treat Cushing’s Syndrome on Lipid Levels
Ketoconazole is used to treat patients with Cushing’s syndrome. It is an anti-fungal imidazole derivative that blocks several steps in cortisol biosynthesis thereby lowering serum cortisol levels. However, ketoconazole is also an inhibitor of cholesterol biosynthesis, acting directly by blocking the conversion of methyl sterols to cholesterol and indirectly by suppressing cholesterol synthesis via feedback inhibition of HMG-CoA reductase by sterol intermediates (269,270). In the past, ketoconazole had been used to treat patients with familial hypercholesterolemia before the widespread use of statins, as it reduced total, intermediate density cholesterol, LDL-C, and apo B levels by approximately 25% (271). Thus, its use to control hypercortisolism may have a beneficial effect on lipid and lipoprotein levels. Levoketoconazole, also decreases total cholesterol and LDL-C levels by approximately 25% and slightly increases HDL-C levels (272).
It is important to recognize that ketoconazole and levoketoconazole also interfere with the metabolism of many drugs through the inhibition of several hepatic P450 enzymes. Simvastatin, lovastatin, and atorvastatin are all metabolized by cytochrome P450 CYP3A4, and thus, their plasma concentrations and risk of myotoxicity are greatly increased with concomitant ketoconazole therapy (273). Pravastatin, pitavastatin, and rosuvastatin are preferable as their plasma concentrations are not significantly increased by CYP3A4 inhibitors (273).
Mitotane is used for treatment of adrenal carcinoma or intractable Cushing’s disease and results in adrenocortical atrophy and necrosis and inhibits steroidogenesis. Mitotane raises circulating cholesterol, LDL-C, Apo B, and HDL-C levels (274-276). Changes in triglyceride levels are variable (276). In one report no changes Lp(a) levels were observed (274). Mitotane increases HMGCoA reductase activity, which may contribute to the increase in LDL-C (277). The increase in LDL-C levels has been shown to be decreased by treatment with statins (274,276). Because mitotane induces CYP3A4 activity one should use a statin that is not metabolized by this enzyme (for example pravastatin or rosuvastatin) (276). In a case report mitotane increased LDL-C levels as high as 300mg/dl (278).
Mifepristone, a potent antagonist of glucocorticoid and progesterone receptors, lowers HDL-C and Apo AI levels (279). The mechanism for this decrease in HDL-C is unknown. In a small study short-term administration of mifepristone reduced serum triglyceride levels, which correlated with increases in adipose tissue lipoprotein lipase activity (280).
Pasireotide is a somatostatin analogue and in patients with Cushing’s syndrome has been shown to decrease total cholesterol and LDL-C levels (281-283). In some studies triglyceride levels were also decreased (282).
TESTOSTERONE
Effect of Testosterone on Lipid and Lipoprotein Levels
ENDOGENOUS TESTOSTERONE LEVELS
Numerous observational (epidemiological) studies have shown that serum testosterone levels directly correlate with HDL-C and Apo A-I levels (i.e. subjects with low serum testosterone levels have lower HDL-C and Apo A-I levels) (284-290). Moreover, low serum testosterone levels are inversely correlated with total cholesterol, LDL-C, Apo B, and triglyceride levels (i.e. subjects with low testosterone levels have higher total cholesterol, LDL-C, Apo B, and triglycerides) (285,289-291). Thus, individuals with low serum testosterone levels have a pro-atherogenic lipoprotein pattern with low HDL-C levels and high triglyceride and LDL-C levels.
Not unexpectedly, given the low HDL-C levels and high triglyceride levels, individuals with low serum testosterone levels are more likely to have the metabolic syndrome (290,292,293). It should be recognized that these associations do not necessarily imply that the low serum testosterone levels are causative. For example, it is likely that obesity and related metabolic abnormalities, such as type 2 diabetes, lead to both the abnormal lipid pattern and the low serum testosterone levels. Indeed, obesity is associated with low testosterone and weight loss restores testosterone levels (293-297). Thus, observational studies may be confounded.
|
Table 9. Correlation of Testosterone Levels with Lipid and Lipoprotein Levels |
|
|
HDL-C |
Positive (low T = lower) |
|
LDL-C |
Negative (low T = higher) |
|
Triglycerides |
Negative (low T = higher) |
|
Non-HDL-C |
Negative (low T = higher) |
|
Lp(a) |
Negative (low T = higher) |
ANDROGEN DEPRIVATION THERAPY
Studies of the effect of androgen deprivation therapy not only constitute a clinically relevant state but also provide an alternative approach to understanding the effects of low testosterone levels on lipid and lipoprotein levels. In contrast to the associations in observational studies, most studies of androgen deprivation therapy have shown an increase in plasma HDL-C and Apo A-I levels (298-305). This increase occurs very rapidly within 2 weeks of lowering serum testosterone levels (298). Furthermore, this increase in HDL-C is inhibited if one simultaneously administers testosterone demonstrating that this increase is due to the suppression of testosterone levels (303). In addition, androgen deprivation therapy is also associated with an elevation of LDL-C, non-HDL-C, Lp(a), and triglyceride levels (299-302,304,306-309). The increase of Lp(a) is notable as the metabolism of Lp(a) often does not parallel the metabolism of LDL.
|
Table 10. Effect of Androgen Deprivation Therapy on Lipid and Lipoprotein Levels |
|
|
HDL-C |
Increase |
|
LDL-C |
Increase |
|
Triglycerides |
Increase |
|
Non-HDL-C |
Increase |
|
Lp(a) |
Increase |
TESTOSTERONE TREATMENT
There have been several meta-analyses that have examined the effect of testosterone treatment on lipid and lipoprotein levels but the results have been variable. Baseline differences, type of therapy, and duration of therapy may contribute to the differing results. A meta-analysis by Whitsel and colleagues demonstrated that total cholesterol, LDL-C, and HDL-C levels decreased after intramuscular testosterone treatment, but triglyceride levels did not change (310). A meta-analysis by Isidori also demonstrated a decrease in HDL-C levels, but found no change in LDL-C with testosterone treatment (both intramuscular and transcutaneous) (311) . Similarly, a meta-analysis by Fernández-Balsells and colleagues demonstrated a decrease in HDL-C levels but no change in LDL-C or triglyceride levels with testosterone treatment (both intramuscular and transcutaneous administration) (312). A meta-analysis by Haddad et al failed to demonstrate any significant changes in HDL-C, LDL-C, or triglyceride levels (313). A recent meta-analysis by Corona and colleagues did not find changes in HDL-C levels but reported small decreases in total cholesterol and triglycerides (314). A meta-analysis of testosterone replacement therapy in patients with type 2 diabetes found a decrease in triglycerides, total cholesterol, and LDL-C and an increase in HDL-C (315). This improvement in lipid parameters could be due to decreases in body weight, glycemic control, and insulin resistance. Finally, a non-randomized long term trial (8 years) of intramuscular testosterone therapy in patients with pre-diabetes resulted in a decrease in body weight and a decrease in A1c that was accompanied by decreases in LDL and non-HDL-C and triglyceride levels and increases in HDL-C levels compared to an untreated comparison group suggesting that long-term therapy might be beneficial on lipids by effecting body weight and glucose homeostasis (316).
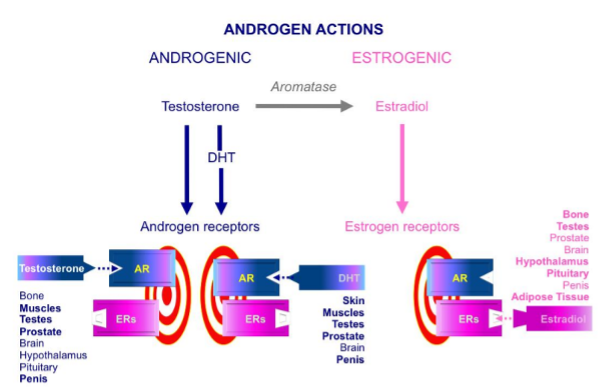
The reason for the differences between these meta-analyses is likely due to the fact that the changes in lipid and lipoprotein levels induced by testosterone treatment are relatively small and variable depending upon the patient population studied, the route and dose of testosterone administration, the duration of therapy, the specific testosterone preparation (whether or not it can undergo aromatization to estrogens), and perhaps other unrecognized factors. For example, the reductions in HDL-C appear to be greater in patients whose baseline HDL-C levels are high (311,312). Additionally, transdermal testosterone treatment appears to have less effect on HDL-C levels than intramuscular administration (317). High dose testosterone treatment appears to more consistently lower HDL-C levels than does low dose treatment (318). For example, testosterone enanthate 200mg IM every week used in a contraception study resulted in a relatively robust 13% decrease in HDL-C levels (319). Similarly, raising serum testosterone levels to higher levels produces greater decreases in LDL-C levels (318). Finally, using testosterone preparations that are not converted to estrogens or simultaneously blocking aromatization can lead to more profound decreases in HDL-C and LDL-C levels, which can be attributed to estrogens having effects on lipid and lipoprotein levels that counterbalance the effects of androgens (estrogens increase HDL-C and decrease LDL-C) (320,321). The important clinical point is that in the typical androgen deficient patients that we treat with the usual testosterone therapy there will only be a modest or no changes in plasma lipid and lipoprotein levels. The minimal effect of testosterone therapy was clearly demonstrated in a large randomized double-blind trial of 788 males over the age of 65 with low testosterone levels who were treated with either testosterone gel to normalize testosterone levels or placebo for 1 year (322). In this trial HDL-C (adjusted mean difference, -2.0 mg/dL; P < 0.001), and LDL-C were both slightly decreased (adjusted mean difference, -2.3 mg/dL; P = 0.051) from baseline with no change in triglyceride levels in the testosterone treated individuals.
While treatment of typical older hypogonadal men with testosterone therapy has only modest to no effects on plasma lipids and lipoproteins, the use of high dose androgenic steroids in young men for the purpose of increasing muscle mass and strength can have profound effects. In a study by Webb and colleagues of 14 individuals taking high dose androgenic steroids, HDL-C levels were markedly reduced to 29mg/dl, which was less than 50% of the mean HDL-C when exogenous steroids were not used (61mg/dl) (323). Additionally in these individuals LDL-C levels were also higher on androgenic steroids (150mg/dl) than off of androgenic steroids (125mg/dl) (323). Similarly, Hurley and colleagues demonstrated that androgen use by eight bodybuilders and four powerlifters lowered HDL-C levels by 55% and raised LDL-C levels by 61% (324). In a double blind cross-over study anabolic steroids, which may not have androgenic effects, induced a 25-27% decrease in HDL-C levels, which returned towards normal 6 weeks after cessation of drug use (325). Thus, if one sees an athletic male with unexpectedly low HDL-C levels one should suspect androgen and/or anabolic steroid use, which is often obtained as a dietary supplement or as a pharmaceutical from an unregulated source.
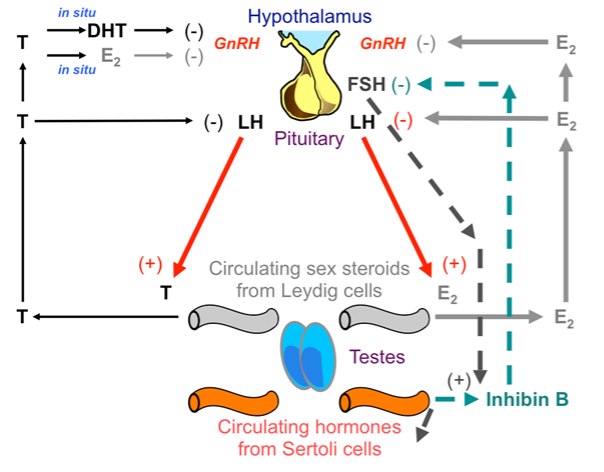
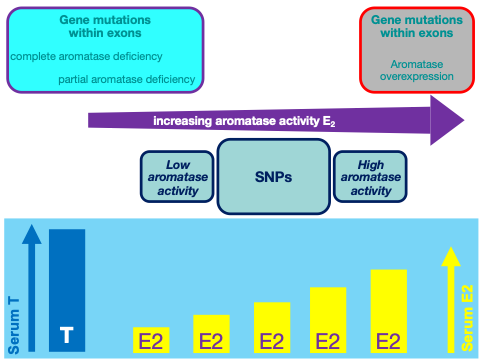
There are a number of potential explanations why the changes in lipid and lipoprotein levels are greater in athletes using androgenic steroids. First, the doses used by the athletes are much higher than used in typical testosterone replacement. Second, the androgenic steroids used are often different and more potent (for example nandrolone-decanoate and oxandrolone). Often the compounds used are not converted to estrogen by aromatase and therefore their effects on serum lipid levels will not be counterbalanced by estrogen formation [265, 272]. Third, aromatase inhibitors are sometimes used simultaneously in combination with the androgenic steroids. Lastly, young athletes are often lean and have little adipose tissue and thus low aromatase activity. There can be individual patient variation in aromatase activity with obese older individuals having increased aromatase activity compared to young athletic individuals (326). As noted earlier, the conversion of testosterone to estrogens by aromatase may blunt the effects of testosterone as estrogens will increase HDL-C levels and decrease LDL-C levels. Together it is likely that these factors account for the more robust changes in lipids and lipoprotein levels induced by androgens in young athletes.
TRANSGENDER MALES
Testosterone therapy in transmen results in an increase in LDL-C levels and a decrease in HDL-C levels with some studies also showing an increase in triglyceride levels (327-331). In transmale adolescents treated with testosterone LDL-C levels increased and HDL-C levels decreased compared to cisgender females (332). These changes are likely due to the combination of an increase in testosterone and a decrease in estrogen.
LIPOPROTEIN (a)
There is a trend towards a higher incidence of clinically significant elevations in Lp(a) levels in men with low testosterone levels (333). Additionally, reductions in serum testosterone levels by orchiectomy or treatment with GnRH antagonists results in an increase in Lp(a) levels (305,334). Conversely, several studies have shown that testosterone administration decreases Lp(a) levels and the effect is more robust in individuals who have high baseline Lp(a) levels (319,335,336). Moreover, it has been shown that simultaneously administering testosterone with an aromatase inhibitor does not markedly reduce the ability of testosterone to decrease Lp(a) levels, indicating that the conversion of testosterone to estrogens does not account for this effect suggesting a direct action of testosterone (335). Lp(a) is a pro-atherogenic lipoprotein so testosterone induced decreases should be beneficial.
SUMMARY
The most consistent effects of androgen therapy on lipid and lipoprotein levels are to decrease HDL-C and Lp(a) levels. These effects are most apparent with high dose testosterone therapy. The decreases in HDL-C and Lp(a) levels with testosterone therapy are consistent with the increases seen with androgen deprivation therapy. However, both types of treatment result in changes that are the opposite of those seen in the observational studies, suggesting that the observational studies are confounded. However, high potency androgen therapy in young healthy men tends to increase LDL-C levels and markedly decrease HDL-C levels (337).
|
Table 11. Effect of Testosterone Therapy on Lipid and Lipoprotein Levels |
|
|
HDL-C |
Decreased or No Change |
|
LDL-C |
Decrease |
|
Triglycerides |
No consistent change |
|
Lp(a) |
Decrease |
Mechanism for the Testosterone Induced Lipid and Lipoprotein Changes
HDL-C
The decrease in HDL-C levels with testosterone administration has been attributed to increases in the expression of SR-B1 in the liver and increases in plasma hepatic lipase activity. In Hep G2 cells, the addition of testosterone increased the mRNA and protein levels of SR-B1 and hepatic lipase but had no effect on the expression of Apo A-I or ABCA1 (338). Moreover, androgen administration increased plasma hepatic lipase activity but had little effect on lipoprotein lipase (320,339-342). An increase in SR-B1 in the liver will facilitate the transfer of cholesterol from HDL particles into the hepatocyte, decreasing plasma HDL-C levels (115). An increase in hepatic lipase activity will increase the hydrolysis of triglycerides and phospholipase on HDL, resulting in the formation of smaller HDL particles, the release of Apo A-I, and increased Apo A-I degradation leading to a decrease in plasma HDL levels (115). Thus, the increase in SR-B1 and hepatic lipase induced by androgens could account for the decrease in HDL-C levels seen with testosterone treatment. There is the potential that the increase in SR-B1 is protective in atherosclerosis as it enhances reverse cholesterol transport from HDL (115).
LDL-C
The mechanism by which testosterone therapy might affect LDL-C levels is uncertain. It has been shown that testosterone can antagonize the ability of estrogens to stimulate LDL receptor expression in the liver, which could lead to a decrease in hepatic LDL receptors and an increase in plasma LDL-C levels (343).
LIPOPROTEIN (a)
The mechanism by which testosterone treatment lowers Lp(a) levels is unknown.
Risk of Cardiovascular Disease
In the Endocrinology of Male Reproduction section of Endotext the chapter by Yeap and Dwivedi (“Androgens and Cardiovascular Disease in Men”), extensively reviews the literature on the linkage of testosterone and cardiovascular disease (344). Therefore, we will only briefly summarize the relevant information.
ENDOGENOUS TESTOSTERONE LEVELS
There have been numerous cross-sectional studies of testosterone levels in patients with coronary artery disease vs. controls and the results have varied (344). Some studies have shown no association while other studies have found low testosterone levels in patients with coronary artery disease. The majority of prospective studies have shown that cardiovascular disease occurs more frequently in subjects with low testosterone levels. Whether the low testosterone is causative or a biomarker of poor cardiovascular health (e.g., obesity, metabolic syndrome, diabetes) cannot be determined from these types of observational studies.
ANDROGEN DEPRIVATION THERAPY
In a meta-analysis by Zhao and colleagues of population-based observational studies comparing androgen deprivation therapy in patients with prostate cancer vs. controls with prostate cancer, six studies were identified with a total of 129,802 androgen deprivation therapy patients and 165,605 controls (345). In this analysis, cardiovascular disease was increased by 10% and cardiovascular mortality by 17% in the androgen deprivation therapy patients. In a meta-analysis by Carneiro and colleagues of 126,898 prostate cancer patients in four cohort studies and 10,760 prostate cancer patients in nine randomized controlled trials, these authors found that cardiovascular events were increased two fold in the androgen deprivation groups (346). When only the randomized trials were analyzed, the relative risk was increased 1.55-fold in the androgen deprivation patients. In contrast, a meta-analysis by Nguyen and colleagues of 8 randomized trials with 4141 patients did not find an increased risk of cardiovascular disease (347). Finally, a meta-analysis by Bosco of eight observational studies reported a relative risk of 1.57 for fatal and non-fatal cardiovascular disease in patients with prostate cancer treated with GnRH agonists (348). These and other results suggest that the risk of cardiovascular disease is increased in men undergoing androgen deprivation therapy, despite the increase in HDL-C.
TESTOSTERONE TREATMENT
There have been a large number of observational studies of the risk of cardiovascular disease in men treated with testosterone replacement and the results have been inconsistent, with some studies showing that testosterone increases the risk while other studies have shown no increase in risk (344). Interestingly, in a very large retrospective study of 544,115 testosterone treated patients it was reported that men treated with intramuscular testosterone had an increased risk of cardiovascular events (1.26) and death (1.34), whereas individuals treated with either testosterone gel or patch did not have an increased risk (349).
With regards to randomized trials, the Testosterone in Older Men with Mobility Limitations Trial (TOM trial) reported an increase in cardiovascular events with testosterone treatment (350). This trial studied 209 men with an average age of 74 years who had a high baseline prevalence of cardiovascular disease (53%) and major cardiovascular risk factors (diabetes 24%, hypertension 85%, and hyperlipidemia 63%). In this trail subjects were treated with high doses of testosterone gel that resulted in high serum testosterone levels. Although 23 subjects in the testosterone group and 5 in the placebo group had a cardiovascular-related adverse event, it should be recognized that many of these cardiovascular events were not atherosclerotic; only 7 men in the testosterone group and 1 in the placebo group had an atherosclerosis related event. Of note, a similar trial using lower doses of testosterone did not observe an increase in cardiovascular events (351). Additionally, a recent randomized trial with 308 men 60 years or older with low or low-normal testosterone levels demonstrated that treatment with testosterone gel for 3 years did not result in a significant difference in the rates of increase in either common carotid artery intima-media thickness or coronary artery calcium (352). In contrast, a randomized trial demonstrated that testosterone treatment compared with placebo was associated with a significantly greater increase in noncalcified plaque volume from baseline to 12 months (from median values of 204 mm3 to 232 mm3 vs 317 mm3 to 325 mm3, respectively; estimated mean difference, 41 mm3; 95% CI, 14 to 67 mm3; P = .003) with no difference in progression of coronary calcium scores (353). It should be noted that baseline plaque volume differed between the testosterone and placebo group, which complicates interpretation of these results.
With the exception of one meta-analysis by Xu et al (354), most meta-analyses of randomized clinical trials of testosterone therapy have not demonstrated a statistically significant difference in the occurrence of cardiovascular events (312,313,355-362). Of note, one meta-analysis explored the effect of the route of administration of testosterone and reported that oral testosterone treatment significantly increased cardiovascular risk (RR = 2.20), while neither intramuscular nor transcutaneous delivery (gel or patch) significantly altered cardiovascular risk (355).
To definitively determine the effect of testosterone replacement therapy on cardiovascular disease will require a large randomized outcome trial similar to the Women’s Health Initiative. The TRAVERSE study is a large randomized trial designed to definitively answer this crucial question (363)
SUMMARY
While the data suggests that androgen deprivation therapy increases the risk of atherosclerotic cardiovascular disease, the effect of testosterone administration is unclear.
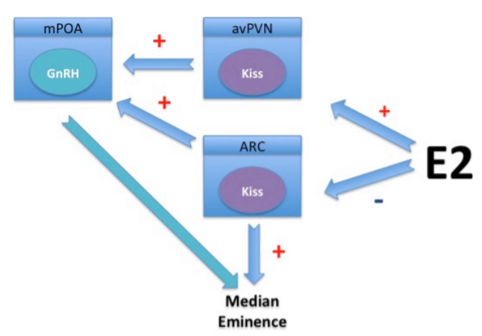
FEMALE SEX STEROID HORMONES
Effect of Female Sex Steroid Hormone on Lipid and Lipoprotein Levels
PREMENOPAUSAL WOMEN
The plasma lipid profile of premenopausal women is less pro-atherogenic than the lipid profile in men (364-367). Specifically, HDL-C levels are increased (approximately 10mg/dl higher in women), while LDL-C and non-HDL-C levels are slightly lower compared to male values (364-367). Additionally plasma triglyceride levels are also decreased and the average size of LDL particles is increased in premenopausal women compared to men (364-367).
Notably most of these differences emerge during puberty. Prior to puberty the lipid profiles of girls and boys are very similar but during puberty HDL-C levels in boys decrease while in girls the HDL-C levels do not change (364-367). Additionally, during puberty triglyceride levels increase in boys with no change in triglyceride levels occurring in girls. LDL-C levels are similar in boys and girls before and during puberty but after age 20 LDL-C increase in both males and females but the increase is greater in males resulting in a modest difference in LDL-C levels between the sexes (364-367).
|
Table 12. Comparison of Lipid and Lipoprotein Levels in Premenopausal Women Compared to Men |
|
|
Lipids/Lipoprotein |
Premenopausal Women Compared to Men |
|
LDL-C |
Lower |
|
HDL-C |
Higher |
|
Triglycerides |
Lower |
|
Non-HDL-C |
Lower |
POSTMENOPAUSAL WOMEN
The changes in lipids and lipoproteins that occur during menopause are relatively small and therefore the results reported in the literature are variable (364-367). Cross-sectional studies tend to show a greater shift towards a pro-atherogenic lipid profile after the menopause whereas in longitudinal studies the changes are smaller (364-367). In post-menopausal women increases in LDL-C are reported in most, but not all studies, and the composition of LDL shifts towards smaller dense LDL particles (364-367). HDL-C levels tend to be stable but some studies have reported small decreases (364-367). Following surgical menopause the above changes tend to be more rapid and robust and in this setting Lp(a) levels have been reported to increase; however, during natural menopause the change in Lp(a) is very modest (368,369). It is important to recognize that during menopause there are changes in factors in addition to the loss of sex steroid hormones that can alter lipid and lipoprotein levels. Menopause is associated with increases in total and central body fat and a decrease in insulin sensitivity, which are well recognized to affect lipid and lipoprotein metabolism (37).
|
Table 13. Effects of Menopause on Lipid and Lipoproteins |
|
|
Lipids/Lipoproteins |
Postmenopausal vs Premenopausal |
|
LDL-C |
Increase |
|
HDL-C |
No change or small decrease |
|
Lp(a) |
No change or increase |
TRANSGENDER FEMALES
In a systemic review and meta-analysis it was reported that in male-to-female individuals, serum TG levels were increased without changes in LDL or HDL-C levels (329). A large observational study of 170 trans females reported an increase in both triglycerides and HDL-C levels (330) but another study only reported an increase in HDL-C levels (331). Additional studies measuring changes in lipid levels in transgender females controlling for estrogen dose, preparation and route of administration, use of other gender affirming therapies, and adjusting for baseline lipid levels are required to better define the changes in lipids that occur.
ESTROGEN TREATMENT
The effects of oral estrogen treatment on lipids and lipoproteins have been recognized for many years (364,366,370,371). Estrogen administration increases HDL-C levels by 5-15% and decreases LDL-C levels by 5-20% (364,366,370,371). In addition, estrogens also increase triglycerides but in patients with genetic or acquired abnormalities in triglyceride metabolism estrogen therapy can precipitate marked hypertriglyceridemia and even the chylomicronemia syndrome (372). In women with normal baseline triglycerides an approximate 10-15mg/dl increase in triglycerides occurs with estrogen therapy (364,366,370,371). If the increase in triglycerides is substantial, it leads to a decrease in LDL size (i.e., formation of small dense LDL). Not unexpectedly, estrogens induce an increase in Apo A-I levels and a decrease in Apo B levels. Lp(a) levels are also decreased by 20-25% by estrogen therapy (364,366,370,371). The effects of oral estradiol are similar to that of oral conjugated equine estrogens (Premarin).
|
Table 14. Effect of Oral Estrogen Treatment on Lipid and Lipoproteins |
|
|
Lipids/Lipoproteins |
Estrogen Treatment |
|
LDL-C |
Decrease |
|
HDL-C |
Increase |
|
Triglycerides |
Increase |
|
Lp(a) |
Decrease |
Transdermal estrogen administration has less of an effect on lipid and lipoproteins (364,366,370,371,373). The increase in HDL-C and the decrease in LDL-C are markedly blunted (364,366,370,371,373). Importantly, the effect of transdermal estrogen on triglycerides is minimal and therefore in patients with baseline abnormalities in triglyceride metabolism, the use of transdermal estrogen therapy is preferred (364,366,370,371,373). In some studies, treatment with transdermal estradiol has actually decreased plasma triglyceride levels (374). The lack of a robust effect on lipids with transdermal estrogen preparations is likely due to decreased exposure of the liver to estrogens compared with oral therapy.
ESTROGEN AND PROGESTERONE TREATMENT
Progestins generally have androgen like effects on lipid and lipoproteins and therefore progestin administration decreases HDL-C and triglyceride levels but has little or no effect on LDL-C levels (364,366,370,371). Thus, when combined with estrogen therapy, the estrogen/progesterone preparation blunts the characteristic estrogen induced increase in HDL-C levels without affecting the estrogen induced reduction in LDL-C levels (364,366,370,371). In many but not all studies, progesterone also blunts the estrogen induced increase in triglyceride levels (364,366,370,371,375). In contrast, progesterone appears to either slightly augment or have no effect on the ability of estrogens to decrease Lp(a) levels (370). It is important to note that the effect of adding progesterone is dependent on both the dose and the androgenicity of the particular progesterone used. Godsland analyzed a large number of studies and found in order of least to most potent progesterone affecting lipid levels the following; dydrogesterone and medrogestone, progesterone, cyproterone acetate, medroxyprogesterone acetate, transdermal norethindrone acetate, norgestrel, and oral norethindrone acetate (370).
The Postmenopausal Estrogen/Progestin Intervention (PEPI) trial randomly assigned 875 healthy postmenopausal women to 1) placebo; (2) conjugated equine estrogen (CEE), 0.625 mg/d; (3) CEE, 0.625 mg/d plus cyclic medroxyprogesterone acetate (MPA), 10 mg/d for 12 days/month; (4) CEE, 0.625 mg/d plus continuous MPA, 2.5 mg/day; or (5) CEE, 0.625 mg/d plus cyclic micronized progesterone (MP), 200 mg/day for 12 days/month (375). The effects on plasma lipid and lipoproteins are shown in table 15, which demonstrates that the addition of medroxyprogesterone but not progesterone blunts the estrogen induced increase in HDL-C without affecting the decrease in LDL-C levels. In this particular study medroxyprogesterone did not blunt the estrogen induced increase in triglyceride levels.
|
Table 15. The Effect of Estrogen with or without Progesterone on Plasma Lipid and Lipoprotein Levels (PEPI Trial) |
|||||
|
|
Placebo |
CEE only |
CEE+MPA (cyc) |
CEE+MPA (con) |
CEE+MP (cyc) |
|
HDL-C |
-1.2% |
5.6% |
1.6% |
1.2% |
4.1% |
|
LDL-C |
-4.1% |
-14.5% |
-17.7% |
-16.5% |
-14.8% |
|
Triglycerides |
-3.2% |
13.7% |
12.7% |
11.4 |
13.4% |
Another study evaluated the effect of hormone replacement on lipid and lipoprotein levels in women with hyperlipidemia (376). In that study, 58 women with a baseline total cholesterol level of 305mg/dl and LDL-C of 212mg/dl were randomly assigned to treatment with 1.25 mg conjugated estrogen plus medroxyprogesterone acetate 5 mg/day or simvastatin 10 mg daily. The results of this trial are shown in table 16 and demonstrate that statins are more effective in lowering LDL-C levels and have a similar effect on HDL-C as hormone replacement therapy. While statins lower triglyceride levels, hormone replacement therapy increases triglycerides. Of note, hormone replacement therapy markedly lowers Lp(a) levels whereas statin treatment has no effect, on this highly atherogenic particle.
|
Table 16. Effect of Hormone Replacement Therapy vs. Statin Treatment on Lipid and Lipoprotein Levels |
||
|
Lipids/Lipoproteins |
Hormone Replacement |
Simvastatin |
|
Total cholesterol |
14% decrease |
26% decrease |
|
LDL-C |
24% decrease |
36% decrease |
|
HDL-C |
7% increase |
7% increase |
|
Triglycerides |
29% increase |
14% decrease |
|
Lp(a) |
27% decrease |
1% increase |
Considerable variation is seen in the response to hormone replacement therapy. This is likely accounted for by different preparations used, route of administration, dosing regimen (cyclic vs. continuous), difference in hormone status prior to treatment, baseline lipid levels, dietary differences, the presence or absence of other metabolic abnormalities, genetic background, etc. (364,370,371). The studies by Tsuda and colleagues showing that the Apo E phenotype influences the response of LDL to hormonal therapy provide an example of how genetic background can influence response (377). Women with the E2/E2 or E2/E3 genotype demonstrated the largest LDL-C decreases while women with the E4/E4 or E4/E3 genotype had only a small change in LDL-C levels in response to hormonal replacement therapy. Another example of the role of genetics are studies showing that polymorphisms of the estrogen receptor-alpha gene may be associated with an augmented HDL-C rise with estrogen therapy (378). It is important to note that women who receive cyclic combined therapy (estrogen and progesterone) may have fluctuations in lipoprotein concentrations depending upon the phase of the cycle and it is therefore important to consistently measure lipids during the same hormonal phase, especially when considering starting medications for hyperlipidemia.
CONTRACEPTIVES
The effect of contraceptives on lipid levels is discussed in the Endotext chapter “Reproductive Health and Its Impact On Lipid Management in Adolescent and Young Adult Females” (379). Table 17 taken from that chapter summarizes the effect of various contraceptives on lipid levels.
|
Table 17. The Effects of Contraceptive Methods on Lipids and Lipoproteins |
||||
|
Contraceptive Method |
LDL-C |
HDL-C |
TG |
Comments |
|
Combined Oral Contraceptive Pill |
||||
|
· Estrogen |
Decrease |
Increase |
Increase |
For OCPs with an identical dose of estrogen, the choice and dose of the progestin component may affect net lipid changes |
|
· Progestin |
Increase |
Decrease |
Decrease |
|
|
Transdermal Patch |
Decrease |
Increase |
Increase |
|
|
Vaginal Ring |
--- |
--- |
Increase |
|
|
DMPA |
Increase |
Decrease |
Neutral |
|
DMPA = Depot medroxyprogesterone acetate
POLYCYSTIC OVARY SYNDROME (PCOS)
Women with PCOS characteristically have low HDL-C levels and increased plasma triglyceride levels (380,381). Additionally, LDL-C and non-HDL-C levels are also increased with the LDL being predominantly small dense LDL (380,381). A meta-analysis of 24 studies reported that in women with PCOS triglyceride levels were increased by 26mg/dl, LDL-C by 12mg/dl, non-HDL-C by 19mg/dl and HDL-C was decreased by 6mg/dl (382). The prevalence of elevated Lp(a) levels is also increased in women with PCOS (380,381). It should be noted that the lipid changes in women with PCOS are observed even when the women are not overweight or obese (380,381). In studies of age and weight matched women, the women with PCOS still have lower HDL-C levels and increased triglycerides, LDL-C, and non-HDL-C levels compared to the controls (380,381). The lipid abnormalities in PCOS are likely multifactorial with increases in androgens, decreases in estrogens, obesity, alterations in fat location, insulin resistance, alterations in glucose homeostasis, genetics, and perhaps other factors all contributing to the lipid abnormalities (380,381). Serum PCSK9 concentrations were higher in PCOS patients than normal controls, which could contribute to the increase in LDL-C levels (383). Angiopoietin-like protein 3 levels were increased in PCOS and could contribute to the increase in triglyceride levels (384).
|
Table 18. Lipid and Lipoprotein Levels in Polycystic Ovarian Syndrome |
|
|
LDL-C |
Increase |
|
HDL-C |
Decrease |
|
Triglycerides |
Increase |
|
Non-HDL-C |
Increase |
|
Lp(a) |
Increase |
Mechanisms for the Female Sex Steroid Induced Lipid and Lipoprotein Changes
ESTROGENS
There are several effects of estrogen that could lead to an increase in HDL-C levels. First, studies have shown that estrogens stimulate the expression of Apo A-I, which will lead to an increased synthesis of Apo A-I and the increased formation of HDL (366,385-389). Second, estrogen therapy decreases hepatic lipase activity, which will decrease the hydrolysis of triglyceride and phospholipids on HDL particles, which could potentially result in a decrease in the catabolism of HDL (390-392). Finally, estrogens suppress the expression of SR-B1 in the liver, which will decrease the transfer of cholesterol from HDL particles into the hepatocyte increasing plasma HDL-C levels (393). Based on kinetic studies it is likely that the predominant effect of estrogens is to increase the production of HDL, which is mediated by an increase in Apo A-I production (366,385-389). The net result may be protective from atherosclerosis.
The decrease in LDL-C induced by estrogen treatment is accounted for by an increase in LDL clearance (366,394-397). Studies have shown that estrogens increase the expression of hepatic LDL receptors (398-401). Additionally, estrogens reduce PCSK9 levels, which would decrease the degradation of LDL receptors (402-404). Together, this would increase the number of hepatic LDL receptors leading to the accelerated clearance of LDL and a reduction in plasma LDL-C levels.
The increase in plasma triglyceride levels induced by estrogen treatment is due to the increased production and secretion of VLDL particles (366,388,397,405-407). The mechanism by which estrogens decrease Lp(a) levels is unknown.
PROGESTINS
Many of the adverse effects of progestins on lipid and lipoproteins, such as decreasing HDL-C levels, are thought to be due to activation of the androgen receptor (i.e. androgenic actions) (408). The considerable variation of progestins in influencing lipid and lipoprotein metabolism are related to their androgenic potency. For detailed information on the effect of testosterone and other androgens on lipid and lipoprotein metabolism see the section above on the mechanism for the testosterone induced lipid and lipoprotein changes.
Risk of Cardiovascular Disease
PREMENOPAUSAL WOMEN
It has been recognized for many years that the risk of cardiovascular disease in premenopausal women is very low and substantially lower than in men of similar age (409-411). There is an approximate 10-year delay in the development of cardiovascular disease in women compared to men. The relative contribution of the less pro-atherogenic lipid profile in women to this sex difference in cardiovascular disease risk is likely important but remains uncertain.
POSTMENOPAUSAL WOMEN
After the menopause, the risk of cardiovascular disease increases in women (409,410). Of particular note, premature menopause is associated with an increased risk of developing cardiovascular disease, indicating that age is not the sole factor contributing to the increased risk in postmenopausal women (412-415).
PREMATURE MENOPAUSE
In a meta-analysis of 15 observational studies with 301,438 women it was reported that the risk of cardiovascular disease was higher in women who had premature menopause (age <40 years; HR 1.55, 95% CI 1.38-1.73; p<0·0001), early menopause (age 40-44 years; 1.30, 1.22-1.39; p<0·0001), and relatively early menopause (age 45-49 years; 1.12, 1.07-1.18; p<0·0001) compared to women who had menopause at 50-51 years of age (416). Similarly, a study of 144,260 women using the UK BioBank found that the risk of coronary artery disease was increased in both women with natural premature menopause and surgical premature menopause compared to women with menopause > 40 years of age (surgical premature menopause HR 2.52, p<.001 and natural premature menopause HR 1.39, p< .02). The above studies and others (417-419) indicate the need to evaluate lipids and other cardiovascular disease risk factors in women with premature menopause.
HORMONE REPLACEMENT THERAPY
Numerous observational studies have suggested that hormone replacement therapy reduces the risk of cardiovascular disease (420-426). Based on those data, therapeutic trials of hormone replacement therapy were undertaken to see if therapy would prevent or decrease cardiovascular disease. Surprisingly, the randomized clinical trial outcome studies have not demonstrated a uniform decrease in cardiovascular events.
HERS Trial
The HERS trial was a randomized, blinded, placebo-controlled secondary prevention trial in 2763 women with known coronary artery disease who were postmenopausal with an intact uterus, with a mean age of 66.7 years (427). Patients were randomized to either 0.625 mg of conjugated equine estrogens plus continuous 2.5 mg of medroxyprogesterone acetate or placebo with an average duration of follow-up of 4.1 years. As expected, LDL-C levels were decreased by 11% and HDL-C levels were increased by 10% in the hormone treated group. Despite these changes, there were no significant differences between the groups in the primary outcome (nonfatal myocardial infarction or CHD death) or in any of the secondary cardiovascular outcomes (coronary revascularization, unstable angina, congestive heart failure, resuscitated cardiac arrest, stroke or transient ischemic attack, and peripheral arterial disease). Interestingly, there were more CHD events in the hormone group in year 1 but fewer in years 4 and 5 compared to the placebo group. An unblinded extension of the HERS trial for an additional 2.7 years (HERSII) found that the lower rates of CHD events among women in the hormone group in the final years of HERS did not persist during additional years of follow-up. After 6.8 years, hormone therapy did not reduce the risk of cardiovascular events in women with pre-existing cardiovascular disease (428). As expected, hormone therapy decreased Lp(a) levels and in a post hoc analysis there was a suggestion that individuals with high baseline Lp(a) levels and individuals who had a robust decrease in Lp(a) with hormone therapy had a reduction in cardiovascular events (429). Of course, these results are not definitive and suggest the need for further focused trials of hormone therapy in postmenopausal women with elevated Lp(a) levels.
Women’s Health Initiative- Estrogen/Progesterone Therapy
The Women’s Health Initiative (WHI) examined the effect of hormone replacement therapy in women with and without an intact uterus. The WHI included a randomized primary-prevention trial of conjugated equine estrogens (CEE) (0.625 mg per day) plus continuous medroxyprogesterone acetate (MPA) (2.5 mg per day) or placebo in 16,608 postmenopausal women with an intact uterus who were 50 to 79 years of age at base line (430). As expected, hormone therapy lowered LDL-C levels by 12.7% and increased HDL-C levels by 7.3% and triglycerides by 6.9%. Despite these changes, after a mean follow-up of 5.2 years (planned duration, 8.5 years), the data and safety monitoring board recommended terminating the trial because the overall risks exceeded the benefits. Combined hormone therapy was associated with a hazard ratio for nonfatal myocardial infarction or death due to CHD of 1.24 in the hormone treated group. Similar to the HERS trial an increased risk of cardiovascular events was greatest in the first year of hormone therapy (HR 1.81).
Women’s Health Initiative- Estrogen Alone Therapy
In women without a uterus, the WHI carried out a randomized, double-blind, placebo-controlled trial of 0.625mg per day of conjugated equine estrogen (CEE) or placebo in 10,739 postmenopausal women, aged 50-79 years of age (431). As expected, the CEE group demonstrated a significant decrease in LDL-C compared to placebo group (−13.7% vs –1.0%, P<.001) and a much larger increase in HDL-C (15.1% vs 1.1%, P<.001). Additionally, large increases in triglyceride levels were observed in the CEE group (25.0% vs 3.0%, P<.001). After an average follow-up of 6.8 years, the estimated hazard ratio for nonfatal myocardial infarction or CHD death in the CEE vs placebo was 0.91 (0.75-1.12). However, the incidence of stroke was increased by 39% in the CEE group (P=.007).
These two initial reports of the results of the WHI coupled with the HERS trial indicated that hormone replacement therapy was not effective in reducing atherosclerotic cardiovascular disease events in a broad spectrum of postmenopausal women.
Women’s Health Initiative- Extension
In 2013 a report was published that extended the follow-up of both the estrogen alone and the combined estrogen/progesterone protocols of the WHI to 13 years (432). It should be noted that after the intervention phase ended only a very small percentage of subjects continued hormonal therapy (<4%). During the cumulative 13-year follow-up, the hazard ratios for nonfatal myocardial infarction or coronary death were 1.09 for CEE plus MPA and 0.94 for CEE alone compared with the placebo groups (both NS). During the 13-year follow-up the hazard ratios for stroke were higher in the hormone therapy groups compared with the placebo groups (HR, 1.16 for CEE plus MPA; HR, 1.15 for CEE alone). Although with cessation of hormonal therapy the risk of atherosclerotic cardiovascular disease appeared to diminish, due to the open label nature of this analysis these data are difficult to interpret. Notably, there was no evidence for a “legacy effect” of cardiovascular benefit or harm after discontinuing hormone therapy. Thus, even with longer follow-up hormonal therapy did not demonstrate a reduction in atherosclerotic cardiovascular disease.
The Subject Age or Time Since Menopause Hypothesis
The WHI results, coupled with those of the HERS trial, have been translated into a recommendation that hormone replacement therapy not be used for cardiovascular disease prevention, that it not be started unless needed for postmenopausal symptom relief, and that it be terminated as soon as possible after obtaining symptom relief. This official interpretation is not accepted, however, by some gynecologists and lipidologists because studies have suggested a more nuanced approach (433). For example, further analysis of the WHI results have suggested that age and/or time from menopause influences the effect of hormonal therapy on atherosclerotic cardiovascular disease events (432). In individuals 50-59 years of age who started hormone treatment with estrogen alone, there was a 40% reduction in coronary heart disease that was borderline statistically significant (p=0.08). In older individuals treated with estrogen alone there was no reduction or even a slight increase in coronary heart disease. In the 50-59 years of age group on estrogen alone, there was a 45% reduction in myocardial infarctions whereas in the 70-79 years of age group, there was a 24% increase in events. In the estrogen-progestin trial the age effect was not observed (Table 19).
|
Table 19. Effect of Age of Starting Hormone Therapy on Coronary Events in Women’s Health Initiative |
||
|
Endpoint and Age at Study Entry |
Estrogen-Progestin |
Estrogen Alone |
|
|
Relative Risk |
Relative Risk |
|
Coronary Heart Disease |
|
|
|
50-59yrs |
1.34 |
0.60 |
|
60-69yrs |
1.01 |
0.95 |
|
70-79yrs |
1.31 |
1.09 |
|
Myocardial Infarction |
|
|
|
50-59yrs |
1.32 |
0.55 |
|
60-69yrs |
1.05 |
0.95 |
|
70-79yrs |
1.46 |
1.24 |
|
Coronary Revascularization |
|
|
|
50-59yrs |
1.03 |
0.56 |
|
60-69yrs |
0.85 |
1.13 |
|
70-79yrs |
1.08 |
1.07 |
A separate, somewhat different age-subgroup analyses from the WHI showed an increase in both coronary heart disease and stroke only in women who started HRT after age 70, while in those age 60-70, there was an increase in stroke but no change in coronary heart disease (434). In further contrast, in those who started hormone therapy before 60 there was no change in stroke, a trend towards decreased coronary heart disease in the CEE study, a trend towards improved global health index in the CEE study, and a statistically significant decrease in total mortality in both studies combined. In fact, there was a trend towards less harm and/or greater benefit in all major endpoints with decreasing age at treatment onset (434).
The age effect is further supported by a meta-analysis of 23 trials with 39,049 women, which showed that hormone therapy significantly reduced CHD events in younger women (OR 0.68 [confidence interval (C I), 0.48 to 0.96]), but not in older women (OR 1.03 [CI, 0.91 to 1.16]) (435). A Cochrane meta-analysis also found an increased risk of cardiovascular events in older individuals treated with hormone therapy but those who started hormone therapy less than 10 years after the menopause had a decreased risk of coronary heart disease (RR 0.52, 95% CI 0.29 to 0.96) (436). Additionally, a more recent randomized trial in 1006 healthy women aged 45-58 who were recently postmenopausal demonstrated that hormonal therapy decreased an end point of death, myocardial infarction, or heart failure by 39% and myocardial infarction by 55% (437). The more clearly positive results may have been due to inclusion of younger women who were closer to the menopause (average 50 years of age and 0.7 years postmenopausal) than in the WHI study. Taken together, these results suggest that younger women who have recently undergone menopause may have either a decrease or no change in atherosclerotic cardiovascular disease when on hormonal therapy. In contrast, hormonal therapy in older women who have been postmenopausal for many years appears to increase the risk of atherosclerotic cardiovascular disease.
A possible explanation for the effect of age and/or time since menopause on the response to hormonal therapy could be the extent of underlying vascular disease (438). Younger women are more likely to have “healthy” vessels and in these circumstances hormonal therapy is beneficial. In contrast, in older women who may already have underlying atherosclerosis, treatment with hormonal therapy is not beneficial but rather may be harmful. Further support for this hypothesis is provided by subgroup analyses in the WHI showing that women without risk factors for atherosclerosis appear to benefit from hormone therapy (439,440). For example, in women with LDL-C levels less than 130mg/dl or without the metabolic syndrome, hormone therapy is beneficial. However, in women with LDL-C levels greater than 130mg/dl or with the metabolic syndrome, hormone therapy increases the risk of coronary heart disease (Table 20). Furthermore, a high cardiovascular risk score identified women at a higher risk for cardiovascular events with hormone replacement therapy (441).
|
Table 20. Effect of Baseline Risk Factors on Coronary Heart Disease Risk |
||
|
|
Odds Ratio for Hormone Therapy Effect |
P, interaction |
|
LDL-C (mg/dl) |
|
|
|
<130 |
0.66 |
0.03 |
|
>130 |
1.46 |
|
|
LDL/HDL ratio |
|
|
|
<2.5 |
0.60 |
0.002 |
|
>2.5 |
1.73 |
|
|
Metabolic Syndrome |
|
|
|
No |
0.97 |
0.03 |
|
Yes |
2.26 |
|
Apart from these considerations of age at treatment onset, there appears to be a strong temporal pattern of risk for cardiovascular disease relative to the time course of hormone therapy. In both the HERS and WHI studies an increase in cardiovascular events occurred during the first year of hormone therapy followed by a decrease with continued treatment (442). Interestingly, a similar temporal pattern was seen in the observational Nurses’ Health Study (443). One can speculate that the increase in coagulation factors induced by hormone therapy might account for this early increase in cardiovascular events. In a separate but related point, observational studies have shown worse outcomes for women who have stopped hormone therapy vs. those who have continued hormone therapy (421). There has never been a randomized trial of hormone therapy discontinuation vs. continuation of hormone therapy so in patients doing well on hormone therapy it is unclear whether stopping therapy will markedly affect the risk of cardiovascular disease.
EFFECT OF HORMONE THERAPY ON ATHEROSCLEROSIS
Given the absence of definitive results in the clinical outcome studies, further insights may be gained by examining studies of anatomical atherosclerotic changes. Several studies have explored the effect of hormonal therapy on the progression of atherosclerosis measured by quantitative coronary angiography, carotid intima-media thickness (CIMT), or coronary calcium scores (CAC). In patients with pre-existing coronary artery disease, hormone replacement therapy did not affect the progression of coronary atherosclerosis or CIMT (444-447). Another study of healthy menopausal women aged 42 to 58 years between 6 and 36 months from last menses without prior CVD events who had a CAC score less than 50 Agatston units reported that CIMT and CAC changes were not significantly different in the hormonal or placebo groups (448). In contrast, in one study of women without pre-existing atherosclerotic disease, hormone replacement therapy slowed the rate of progression of CIMT (449). These observations support the clinical outcome studies that have shown that women with pre-existing atherosclerotic cardiovascular disease do not benefit from hormone therapy. In contrast, in women without pre-existing atherosclerotic cardiovascular disease, hormone therapy may be beneficial or neutral depending upon the particular study.
In the WHI estrogen alone trial, coronary artery calcium scores were measured in women between 50-59 years of age at study entry (448). The mean coronary-artery calcium score after trial completion was lower in women receiving estrogen therapy (83.1A) than in women receiving placebo (123.1A) (P = 0.02). This indicates that calcified-plaque burden in the coronary arteries was lower in younger women assigned to estrogen also supporting the hypothesis that estrogen therapy reduces the progression of atherosclerosis in women who are recently menopausal and do not have pre-existing atherosclerosis.
Hodis and colleagues randomly assigned 643 healthy postmenopausal women who were stratified according to time since menopause (<6 years [early post-menopause ] or ≥10 years [late post-menopause]) to receive either oral 17β-estradiol plus progesterone for 10 days of each 30-day cycle or placebo (450). In support of the WHI results, in women who were less than 6 years past menopause, the mean CIMT increased by 0.0078 mm per year in the placebo group versus 0.0044 mm per year in the estradiol group (P=0.008) while in women who were 10 or more years past menopause the rate of CIMT progression in the placebo and estradiol groups were similar. Coronary-artery calcium, total stenosis, and plaque did not differ significantly between the placebo group and either early or late postmenopausal group on hormonal therapy. Nevertheless, these observations suggest a difference in response to hormonal replacement therapy depending on duration of time since menopause.
In summary, in older women or women with pre-existing atherosclerosis, the data demonstrates that hormone therapy is not beneficial and is likely harmful. In younger women or women without pre-existing atherosclerosis studies suggest that hormone therapy is either modestly beneficial or neutral.
ORAL CONTRACEPTIVES
A Cochrane review has recently addressed the effect of oral contraceptives on atherosclerotic cardiovascular disease (451). They reported that oral contraceptive use did not increase the risk of myocardial infarction or ischemic stroke compared with non-users. The risks did not vary according to the generation of progestogen or according to progestogen type. However, the risk of myocardial infarction or ischemic stroke appeared to increase with higher doses of estrogen. The risk of myocardial infarction or ischemic stroke was only increased in women using oral contraceptives containing ≥ 50 µg of estrogen. In another meta-analysis of progesterone only contraceptives there did not appear to be an increase in the risk of myocardial infarctions (452). Additionally, another recent meta-analysis reported an increase in ischemic strokes but no increase in myocardial infarctions with oral contraceptive use (453). It should be noted that earlier meta-analyses have reported an increased risk of myocardial infarctions and ischemic strokes, which may be related to differences in the composition of the products and doses being used in the past in oral contraceptives (454,455). Thus, oral contraceptives with higher doses of estrogen likely increase cardiovascular disease risk.
POLYCYSTIC OVARY SYNDROME (PCOS)
A recent meta-analysis of five case-control studies and five cohort studies involving a total of 104,392 subjects found that PCOS was associated with a significant increased risk of cardiovascular disease (OR = 1.30) (456). Another smaller meta-analysis reported a 2-fold risk of arterial disease for patients with PCOS compared to women without PCOS (457). In contrast, in a study of cardiovascular events in 309 women with PCOS vs. 343 women without PCOS followed for a mean duration of 23.7 years an increase in cardiovascular disease was not observed (458). Of note the population of patients with PCOS in this study did not have diabetes or dyslipidemia and their BMI was only slightly greater than the controls (29.4 kg/m2 vs 28.3 kg/m2). In recent reviews it was noted that an increased prevalence of cardiovascular disease in women with PCOS has not been conclusively demonstrated (459,460). It has been proposed that the increased risk of cardiovascular disease in women with PCOS is mainly observed in women who are obese and/or have diabetes (461). A meta-analysis of studies comparing carotid intima-media thickness (CIMT) in individuals with PCOS vs. controls reported that women with PCOS have a higher mean CIMT compared with non-PCOS controls (462) but not all studies have shown this relationship (463). Most but not all studies have shown that women with PCOS have higher coronary calcium scores than controls (463-468). In PCOS it is likely that many factors, such as decreased estrogen levels, increased testosterone levels, insulin resistance, hypertension, obesity, increased inflammation, alterations in glucose homeostasis, etc., could contribute to the increased cardiovascular risk in addition to a pro-atherogenic lipid profile and differences in the prevalence of various cardiovascular risk factors in patients with PCOS could account for the variable risk of cardiovascular events.
MANAGEMENT GUIDELINES
In 2020 the Endocrine Society published guidelines on the treatment of lipid disorders in patients with endocrine disorders (268). These recommendations are summarized in table 21.
|
Table 21. Endocrine Society Guidelines for the Management of Lipids in Patients with Endocrine Diseases |
|
|
GH Deficiency |
Obtain a lipid profile at diagnosis |
|
GH deficiency associated with hypopituitarism |
Assess and treat lipids and other cardiovascular risk factors |
|
Acromegaly |
Measure lipid profile before and after treatment of GH excess |
|
Hypothyroidism |
Suggest against treating hyperlipidemia until the patient is euthyroid |
|
Subclinical hypothyroidism (TSH <10 mIU/L) |
Suggest considering thyroxine treatment to reduce LDL-C levels |
|
Hyperthyroid |
Re-evaluate lipids after the patient becomes euthyroid |
|
Cushing’s syndrome |
Monitor the lipid profile In adults with persistent endogenous Cushing syndrome, we suggest statin therapy (LDL-C > 70mg/dL), to reduce ASCVD risk, irrespective of the risk score |
|
Hypogonadism |
Testosterone as symptomatically indicated, and not to improve dyslipidemia or ASCVD risk. |
|
Polycystic ovary syndrome |
Obtaining a fasting lipid panel at diagnosis to assess ASCVD risk |
|
Menopause and hormonal replacement |
Treat dyslipidemia with statin therapy, rather than hormone therapy. In women who enter menopause early (<40 to 45 years old), we recommend assessment and treatment of lipids and other ASCVD risk factors |
|
Gender-affirming hormone therapy |
In transwomen and transmen who have taken or are taking gender-affirming hormone therapy, assess ASCVD risk by guidelines for non-transgender adults |
GH- Growth Hormone
ACKOWLEDGEMENTS
The author thanks Drs Carl Grunfeld and Eliot Brinton for their help in earlier editions of this chapter.
REFERENCES
- Pala NA, Laway BA, Misgar RA, Dar RA. Metabolic abnormalities in patients with prolactinoma: response to treatment with cabergoline. Diabetol Metab Syndr 2015; 7:99
- Pelkonen R, Nikkila EA, Grahne B. Serum lipids, postheparin plasma lipase activities and glucose tolerance in patients with prolactinoma. Clin Endocrinol (Oxf) 1982; 16:383-390
- Erem C, Kocak M, Nuhoglu I, Yilmaz M, Ucuncu O. Blood coagulation, fibrinolysis and lipid profile in patients with prolactinoma. Clin Endocrinol (Oxf) 2010; 73:502-507
- Oppenheim DS, Greenspan SL, Zervas NT, Schoenfeld DA, Klibanski A. Elevated serum lipids in hypogonadal men with and without hyperprolactinemia. Ann Intern Med 1989; 111:288-292
- Peric B, Kruljac I, Sundalic S, Pecina HI, Jovic A, Stefanovic M, Butorac D, Vrkljan M. Obesity and hypercholesterolemia in patients with prolactinomas: Could DHEA-S and growth hormone be the missing link? Endocr Res 2016; 41:200-206
- Berinder K, Nystrom T, Hoybye C, Hall K, Hulting AL. Insulin sensitivity and lipid profile in prolactinoma patients before and after normalization of prolactin by dopamine agonist therapy. Pituitary 2011; 14:199-207
- Fahy U, Hopton MI, Hartog M, Bolton CH, Hull MG. The lipoprotein profile of women with hyperprolactinaemic amenorrhoea. Hum Reprod 1999; 14:285-287
- Glezer A, Santana MR, Bronstein MD, Donato J, Jr., Jallad RS. The interplay between prolactin and cardiovascular disease. Front Endocrinol (Lausanne) 2022; 13:1018090
- Arslan MS, Topaloglu O, Sahin M, Tutal E, Gungunes A, Cakir E, Ozturk IU, Karbek B, Ucan B, Ginis Z, Cakal E, Ozbek M, Delibasi T. Preclinical atherosclerosis in patients with prolactinoma. Endocr Pract 2014; 20:447-451
- Jiang XB, Li CL, He DS, Mao ZG, Liu DH, Fan X, Hu B, Zhu YH, Wang HJ. Increased carotid intima media thickness is associated with prolactin levels in subjects with untreated prolactinoma: a pilot study. Pituitary2014; 17:232-239
- Heshmati HM, Turpin G, de Gennes JL. Chronic hyperprolactinemia and plasma lipids in women. Klin Wochenschr 1987; 65:516-519
- Ling C, Svensson L, Oden B, Weijdegard B, Eden B, Eden S, Billig H. Identification of functional prolactin (PRL) receptor gene expression: PRL inhibits lipoprotein lipase activity in human white adipose tissue. J Clin Endocrinol Metab 2003; 88:1804-1808
- Auriemma RS, Granieri L, Galdiero M, Simeoli C, Perone Y, Vitale P, Pivonello C, Negri M, Mannarino T, Giordano C, Gasperi M, Colao A, Pivonello R. Effect of cabergoline on metabolism in prolactinomas. Neuroendocrinology 2013; 98:299-310
- Ciresi A, Amato MC, Guarnotta V, Lo Castro F, Giordano C. Higher doses of cabergoline further improve metabolic parameters in patients with prolactinoma regardless of the degree of reduction in prolactin levels. Clin Endocrinol (Oxf) 2013; 79:845-852
- dos Santos Silva CM, Barbosa FR, Lima GA, Warszawski L, Fontes R, Domingues RC, Gadelha MR. BMI and metabolic profile in patients with prolactinoma before and after treatment with dopamine agonists. Obesity (Silver Spring) 2011; 19:800-805
- Inancli SS, Usluogullari A, Ustu Y, Caner S, Tam AA, Ersoy R, Cakir B. Effect of cabergoline on insulin sensitivity, inflammation, and carotid intima media thickness in patients with prolactinoma. Endocrine 2013; 44:193-199
- Byberg S, Futtrup J, Andreassen M, Krogh J. Metabolic effects of dopamine agonists in patients with prolactinomas: a systematic review and meta-analysis. Endocr Connect 2019;
- Schwetz V, Librizzi R, Trummer C, Theiler G, Stiegler C, Pieber TR, Obermayer-Pietsch B, Pilz S. Treatment of hyperprolactinaemia reduces total cholesterol and LDL in patients with prolactinomas. Metab Brain Dis2017; 32:155-161
- Khalil G, Khan FA, Jamal QM, Saleem A, Masroor H, Abbas K. Change in Insulin Sensitivity and Lipid Profile After Dopamine Agonist Therapy in Patients With Prolactinoma. Cureus 2021; 13:e17824
- Kamath V, Jones CN, Yip JC, Varasteh BB, Cincotta AH, Reaven GM, Chen YD. Effects of a quick-release form of bromocriptine (Ergoset) on fasting and postprandial plasma glucose, insulin, lipid, and lipoprotein concentrations in obese nondiabetic hyperinsulinemic women. Diabetes Care 1997; 20:1697-1701
- Pirchio R, Auriemma RS, Solari D, Arnesi M, Pivonello C, Negri M, de Angelis C, Cavallo LM, Cappabianca P, Colao A, Pivonello R. Effects of Pituitary Surgery and High-Dose Cabergoline Therapy on Metabolic Profile in Patients With Prolactinoma Resistant to Conventional Cabergoline Treatment. Front Endocrinol (Lausanne)2021; 12:769744
- Yazici D, Sunbul M, Yasar M, Deyneli O, Yavuz D. Is there an increased cardiovascular risk in patients with prolactinoma? A challenging question. J Clin Ultrasound 2021; 49:870-877
- Haring R, Friedrich N, Volzke H, Vasan RS, Felix SB, Dorr M, Meyer zu Schwabedissen HE, Nauck M, Wallaschofski H. Positive association of serum prolactin concentrations with all-cause and cardiovascular mortality. Eur Heart J 2014; 35:1215-1221
- Carrero JJ, Kyriazis J, Sonmez A, Tzanakis I, Qureshi AR, Stenvinkel P, Saglam M, Stylianou K, Yaman H, Taslipinar A, Vural A, Gok M, Yenicesu M, Daphnis E, Yilmaz MI. Prolactin levels, endothelial dysfunction, and the risk of cardiovascular events and mortality in patients with CKD. Clin J Am Soc Nephrol 2012; 7:207-215
- Krogh J, Selmer C, Torp-Pedersen C, Gislason GH, Kistorp C. Hyperprolactinemia and the Association with All-Cause Mortality and Cardiovascular Mortality. Horm Metab Res 2017; 49:411-417
- Toulis KA, Robbins T, Reddy N, Balachandran K, Gokhale K, Wijesinghe H, Cheng KK, Karavitaki N, Wass J, Nirantharakumar K. Males with prolactinoma are at increased risk of incident cardiovascular disease. Clin Endocrinol (Oxf) 2018; 88:71-76
- Rosen T, Eden S, Larson G, Wilhelmsen L, Bengtsson BA. Cardiovascular risk factors in adult patients with growth hormone deficiency. Acta Endocrinol (Copenh) 1993; 129:195-200
- de Boer H, Blok GJ, Voerman HJ, Phillips M, Schouten JA. Serum lipid levels in growth hormone-deficient men. Metabolism 1994; 43:199-203
- Attanasio AF, Lamberts SW, Matranga AM, Birkett MA, Bates PC, Valk NK, Hilsted J, Bengtsson BA, Strasburger CJ. Adult growth hormone (GH)-deficient patients demonstrate heterogeneity between childhood onset and adult onset before and during human GH treatment. Adult Growth Hormone Deficiency Study Group. J Clin Endocrinol Metab 1997; 82:82-88
- Abdu TA, Neary R, Elhadd TA, Akber M, Clayton RN. Coronary risk in growth hormone deficient hypopituitary adults: increased predicted risk is due largely to lipid profile abnormalities. Clin Endocrinol (Oxf) 2001; 55:209-216
- Rizzo M, Trepp R, Berneis K, Christ ER. Atherogenic lipoprotein phenotype and low-density lipoprotein size and subclasses in patients with growth hormone deficiency before and after short-term replacement therapy. Eur J Endocrinol 2007; 156:361-367
- Thomas JD, Monson JP. Adult GH deficiency throughout lifetime. Eur J Endocrinol 2009; 161 Suppl 1:S97-S106
- Murray RD, Wieringa G, Lawrance JA, Adams JE, Shalet SM. Partial growth hormone deficiency is associated with an adverse cardiovascular risk profile and increased carotid intima-medial thickness. Clin Endocrinol (Oxf)2010; 73:508-515
- Abs R, Feldt-Rasmussen U, Mattsson AF, Monson JP, Bengtsson BA, Goth MI, Wilton P, Koltowska-Haggstrom M. Determinants of cardiovascular risk in 2589 hypopituitary GH-deficient adults - a KIMS database analysis. Eur J Endocrinol 2006; 155:79-90
- Salman S, Uzum AK, Telci A, Alagol F, Ozbey NC. Serum adipokines and low density lipoprotein subfraction profile in hypopituitary patients with growth hormone deficiency. Pituitary 2012; 15:386-392
- O'Neal D, Hew FL, Sikaris K, Ward G, Alford F, Best JD. Low density lipoprotein particle size in hypopituitary adults receiving conventional hormone replacement therapy. J Clin Endocrinol Metab 1996; 81:2448-2454
- Feingold KR, Grunfeld C. Obesity and Dyslipidemia. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- Newman CB, Carmichael JD, Kleinberg DL. Effects of low dose versus high dose human growth hormone on body composition and lipids in adults with GH deficiency: a meta-analysis of placebo-controlled randomized trials. Pituitary 2015; 18:297-305
- Maison P, Griffin S, Nicoue-Beglah M, Haddad N, Balkau B, Chanson P, Metaanalysis of Blinded RP-CT. Impact of growth hormone (GH) treatment on cardiovascular risk factors in GH-deficient adults: a Metaanalysis of Blinded, Randomized, Placebo-Controlled Trials. J Clin Endocrinol Metab 2004; 89:2192-2199
- Gazzaruso C, Gola M, Karamouzis I, Giubbini R, Giustina A. Cardiovascular risk in adult patients with growth hormone (GH) deficiency and following substitution with GH--an update. J Clin Endocrinol Metab 2014; 99:18-29
- Eden S, Wiklund O, Oscarsson J, Rosen T, Bengtsson BA. Growth hormone treatment of growth hormone-deficient adults results in a marked increase in Lp(a) and HDL cholesterol concentrations. Arterioscler Thromb1993; 13:296-301
- Elbornsson M, Gotherstrom G, Bosaeus I, Bengtsson BA, Johannsson G, Svensson J. Fifteen years of GH replacement improves body composition and cardiovascular risk factors. Eur J Endocrinol 2013; 168:745-753
- Monson JP, Jonsson P, Koltowska-Haggstrom M, Kourides I. Growth hormone (GH) replacement decreases serum total and LDL-cholesterol in hypopituitary patients on maintenance HMG CoA reductase inhibitor (statin) therapy. Clin Endocrinol (Oxf) 2007; 67:623-628
- Bengtsson BA, Abs R, Bennmarker H, Monson JP, Feldt-Rasmussen U, Hernberg-Stahl E, Westberg B, Wilton P, Wuster C. The effects of treatment and the individual responsiveness to growth hormone (GH) replacement therapy in 665 GH-deficient adults. KIMS Study Group and the KIMS International Board. J Clin Endocrinol Metab 1999; 84:3929-3935
- Garry P, Collins P, Devlin JG. An open 36-month study of lipid changes with growth hormone in adults: lipid changes following replacement of growth hormone in adult acquired growth hormone deficiency. Eur J Endocrinol 1996; 134:61-66
- Laron Z, Wang XL, Klinger B, Silbergeld A, Wilcken DE. Growth hormone increases and insulin-like growth factor-I decreases circulating lipoprotein(a). Eur J Endocrinol 1997; 136:377-381
- O'Halloran DJ, Wieringa G, Tsatsoulis A, Shalet SM. Increased serum lipoprotein(a) concentrations after growth hormone (GH) treatment in patients with isolated GH deficiency. Ann Clin Biochem 1996; 33 ( Pt 4):330-334
- Weaver JU, Monson JP, Noonan K, John WG, Edwards A, Evans KA, Cunningham J. The effect of low dose recombinant human growth hormone replacement on regional fat distribution, insulin sensitivity, and cardiovascular risk factors in hypopituitary adults. J Clin Endocrinol Metab 1995; 80:153-159
- Fernandez-Perez L, Novoa J, Stahlberg N, Santana-Farre R, Boronat M, Marrero D, Henriquez-Hernandez L, Norstedt G, Flores-Morales A. The effect of in vivo growth hormone treatment on blood gene expression in adults with growth hormone deficiency reveals potential biomarkers to monitor growth hormone therapy. Clin Endocrinol (Oxf) 2010; 72:800-806
- Svensson J, Bengtsson BA, Taskinen MR, Wiklund O, Johannsson G. A nine-month, placebo-controlled study of the effects of growth hormone treatment on lipoproteins and LDL size in abdominally obese men. Growth Horm IGF Res 2000; 10:118-126
- Olivecrona H, Ericsson S, Berglund L, Angelin B. Increased concentrations of serum lipoprotein (a) in response to growth hormone treatment. BMJ 1993; 306:1726-1727
- Laron Z. Increase of serum lipoprotein (a), an adverse effect of growth hormone treatment. Growth Horm IGF Res 2022; 67:101503
- Olivecrona H, Johansson AG, Lindh E, Ljunghall S, Berglund L, Angelin B. Hormonal regulation of serum lipoprotein(a) levels. Contrasting effects of growth hormone and insulin-like growth factor-I. Arteriosclerosis, thrombosis, and vascular biology 1995; 15:847-849
- Parini P, Angelin B, Lobie PE, Norstedt G, Rudling M. Growth hormone specifically stimulates the expression of low density lipoprotein receptors in human hepatoma cells. Endocrinology 1995; 136:3767-3773
- Rudling M, Norstedt G, Olivecrona H, Reihner E, Gustafsson JA, Angelin B. Importance of growth hormone for the induction of hepatic low density lipoprotein receptors. Proc Natl Acad Sci U S A 1992; 89:6983-6987
- Persson L, Cao G, Stahle L, Sjoberg BG, Troutt JS, Konrad RJ, Galman C, Wallen H, Eriksson M, Hafstrom I, Lind S, Dahlin M, Amark P, Angelin B, Rudling M. Circulating proprotein convertase subtilisin kexin type 9 has a diurnal rhythm synchronous with cholesterol synthesis and is reduced by fasting in humans. Arterioscler Thromb Vasc Biol 2010; 30:2666-2672
- Lind S, Rudling M, Ericsson S, Olivecrona H, Eriksson M, Borgstrom B, Eggertsen G, Berglund L, Angelin B. Growth hormone induces low-density lipoprotein clearance but not bile acid synthesis in humans. Arterioscler Thromb Vasc Biol 2004; 24:349-356
- Christ ER, Cummings MH, Jackson N, Stolinski M, Lumb PJ, Wierzbicki AS, Sonksen PH, Russell-Jones DL, Umpleby AM. Effects of growth hormone (GH) replacement therapy on low-density lipoprotein apolipoprotein B100 kinetics in adult patients with GH deficiency: a stable isotope study. J Clin Endocrinol Metab 2004; 89:1801-1807
- Cummings MH, Christ E, Umpleby AM, Albany E, Wierzbicki A, Lumb PJ, Sonksen PH, Russell-Jones DL. Abnormalities of very low density lipoprotein apolipoprotein B-100 metabolism contribute to the dyslipidaemia of adult growth hormone deficiency. J Clin Endocrinol Metab 1997; 82:2010-2013
- Christ ER, Cummings MH, Albany E, Umpleby AM, Lumb PJ, Wierzbicki AS, Naoumova RP, Boroujerdi MA, Sonksen PH, Russell-Jones DL. Effects of growth hormone (GH) replacement therapy on very low density lipoprotein apolipoprotein B100 kinetics in patients with adult GH deficiency: a stable isotope study. J Clin Endocrinol Metab 1999; 84:307-316
- Moller N, Vendelbo MH, Kampmann U, Christensen B, Madsen M, Norrelund H, Jorgensen JO. Growth hormone and protein metabolism. Clin Nutr 2009; 28:597-603
- Moller N, Jorgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocrine reviews 2009; 30:152-177
- Tao R, Acquati F, Marcovina SM, Hobbs HH. Human growth hormone increases apo(a) expression in transgenic mice. Arterioscler Thromb Vasc Biol 1999; 19:2439-2447
- Svensson J, Bengtsson BA, Rosen T, Oden A, Johannsson G. Malignant disease and cardiovascular morbidity in hypopituitary adults with or without growth hormone replacement therapy. J Clin Endocrinol Metab 2004; 89:3306-3312
- Bates AS, Van't Hoff W, Jones PJ, Clayton RN. The effect of hypopituitarism on life expectancy. J Clin Endocrinol Metab 1996; 81:1169-1172
- Erfurth EM, Bulow B, Hagmar LE. Is vascular mortality increased in hypopituitarism? Pituitary 2000; 3:77-81
- Bulow B, Hagmar L, Mikoczy Z, Nordstrom CH, Erfurth EM. Increased cerebrovascular mortality in patients with hypopituitarism. Clin Endocrinol (Oxf) 1997; 46:75-81
- Tomlinson JW, Holden N, Hills RK, Wheatley K, Clayton RN, Bates AS, Sheppard MC, Stewart PM. Association between premature mortality and hypopituitarism. West Midlands Prospective Hypopituitary Study Group. Lancet 2001; 357:425-431
- Stochholm K, Laursen T, Green A, Laurberg P, Andersen M, Kristensen LO, Feldt-Rasmussen U, Christiansen JS, Frydenberg M, Gravholt CH. Morbidity and GH deficiency: a nationwide study. Eur J Endocrinol 2008; 158:447-457
- Cannavo S, Marini F, Curto L, Torre ML, de Gregorio C, Salamone I, Alibrandi A, Trimarchi F. High prevalence of coronary calcifications and increased risk for coronary heart disease in adults with growth hormone deficiency. J Endocrinol Invest 2011; 34:32-37
- Colao A, Di Somma C, Spiezia S, Savastano S, Rota F, Savanelli MC, Lombardi G. Growth hormone treatment on atherosclerosis: results of a 5-year open, prospective, controlled study in male patients with severe growth hormone deficiency. J Clin Endocrinol Metab 2008; 93:3416-3424
- Markussis V, Beshyah SA, Fisher C, Sharp P, Nicolaides AN, Johnston DG. Detection of premature atherosclerosis by high-resolution ultrasonography in symptom-free hypopituitary adults. Lancet 1992; 340:1188-1192
- Benedini S, Dalle Carbonare L, Albiger N, Scanarini M, Bilora F, Petrobelli F, Giannini S, Mantero F, Scaroni C. Effect of short-term therapy with recombinant human growth hormone (GH) on metabolic parameters and preclinical atherosclerotic markers in hypopituitary patients with growth hormone deficiency. Horm Metab Res2006; 38:16-21
- Colao A, Di Somma C, Cuocolo A, Spinelli L, Acampa W, Spiezia S, Rota F, Savanelli MC, Lombardi G. Does a gender-related effect of growth hormone (GH) replacement exist on cardiovascular risk factors, cardiac morphology, and performance and atherosclerosis? Results of a two-year open, prospective study in young adult men and women with severe GH deficiency. J Clin Endocrinol Metab 2005; 90:5146-5155
- Soares DV, Spina LD, de Lima Oliveira Brasil RR, da Silva EM, Lobo PM, Salles E, Coeli CM, Conceicao FL, Vaisman M. Carotid artery intima-media thickness and lipid profile in adults with growth hormone deficiency after long-term growth hormone replacement. Metabolism 2005; 54:321-329
- Murata M, Kaji H, Mizuno I, Sakurai T, Iida K, Okimura Y, Chihara K. A study of carotid intima-media thickness in GH-deficient Japanese adults during onset among adults and children. Eur J Endocrinol 2003; 148:333-338
- Pfeifer M, Verhovec R, Zizek B, Prezelj J, Poredos P, Clayton RN. Growth hormone (GH) treatment reverses early atherosclerotic changes in GH-deficient adults. J Clin Endocrinol Metab 1999; 84:453-457
- Bengtsson BA, Koppeschaar HP, Abs R, Bennmarker H, Hernberg-Stahl E, Westberg B, Wilton P, Monson JP, Feldt-Rasmussen U, Wuster C. Growth hormone replacement therapy is not associated with any increase in mortality. KIMS Study Group. J Clin Endocrinol Metab 1999; 84:4291-4292
- Holmer H, Svensson J, Rylander L, Johannsson G, Rosen T, Bengtsson BA, Thoren M, Hoybye C, Degerblad M, Bramnert M, Hagg E, Eden Engstrom B, Ekman B, Norrving B, Hagmar L, Erfurth EM. Nonfatal stroke, cardiac disease, and diabetes mellitus in hypopituitary patients on hormone replacement including growth hormone. J Clin Endocrinol Metab 2007; 92:3560-3567
- van Bunderen CC, van Nieuwpoort IC, Arwert LI, Heymans MW, Franken AA, Koppeschaar HP, van der Lely AJ, Drent ML. Does growth hormone replacement therapy reduce mortality in adults with growth hormone deficiency? Data from the Dutch National Registry of Growth Hormone Treatment in adults. J Clin Endocrinol Metab 2011; 96:3151-3159
- Borson-Chazot F, Serusclat A, Kalfallah Y, Ducottet X, Sassolas G, Bernard S, Labrousse F, Pastene J, Sassolas A, Roux Y, Berthezene F. Decrease in carotid intima-media thickness after one year growth hormone (GH) treatment in adults with GH deficiency. J Clin Endocrinol Metab 1999; 84:1329-1333
- Cenci MC, Conceicao FL, Soares DV, Spina LD, Brasil RR, Lobo PM, Michmacher E, Vaisman M. Impact of 5 years of growth hormone replacement therapy on cardiovascular risk factors in growth hormone-deficient adults. Metabolism 2008; 57:121-129
- Gibney J, Wallace JD, Spinks T, Schnorr L, Ranicar A, Cuneo RC, Lockhart S, Burnand KG, Salomon F, Sonksen PH, Russell-Jones D. The effects of 10 years of recombinant human growth hormone (GH) in adult GH-deficient patients. J Clin Endocrinol Metab 1999; 84:2596-2602
- Oliveira JL, Aguiar-Oliveira MH, D'Oliveira A, Jr., Pereira RM, Oliveira CR, Farias CT, Barreto-Filho JA, Anjos-Andrade FD, Marques-Santos C, Nascimento-Junior AC, Alves EO, Oliveira FT, Campos VC, Ximenes R, Blackford A, Parmigiani G, Salvatori R. Congenital growth hormone (GH) deficiency and atherosclerosis: effects of GH replacement in GH-naive adults. J Clin Endocrinol Metab 2007; 92:4664-4670
- Vilar L, Naves LA, Costa SS, Abdalla LF, Coelho CE, Casulari LA. Increase of classic and nonclassic cardiovascular risk factors in patients with acromegaly. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists 2007; 13:363-372
- Takeda R, Tatami R, Ueda K, Sagara H, Nakabayashi H, Mabuchi H. The incidence and pathogenesis of hyperlipidaemia in 16 consecutive acromegalic patients. Acta endocrinologica 1982; 100:358-362
- Nikkila EA, Pelkonen R. Serum lipids in acromegaly. Metabolism: clinical and experimental 1975; 24:829-838
- Landin-Wilhelmsen K, Tengborn L, Wilhelmsen L, Bengtsson BA. Elevated fibrinogen levels decrease following treatment of acromegaly. Clinical endocrinology 1997; 46:69-74
- Colao A, Marzullo P, Lombardi G. Effect of a six-month treatment with lanreotide on cardiovascular risk factors and arterial intima-media thickness in patients with acromegaly. European journal of endocrinology / European Federation of Endocrine Societies 2002; 146:303-309
- Colao A, Spinelli L, Cuocolo A, Spiezia S, Pivonello R, di Somma C, Bonaduce D, Salvatore M, Lombardi G. Cardiovascular consequences of early-onset growth hormone excess. The Journal of clinical endocrinology and metabolism 2002; 87:3097-3104
- Colao A, Pivonello R, Grasso LF, Auriemma RS, Galdiero M, Savastano S, Lombardi G. Determinants of cardiac disease in newly diagnosed patients with acromegaly: results of a 10 year survey study. European journal of endocrinology / European Federation of Endocrine Societies 2011; 165:713-721
- Boero L, Manavela M, Gomez Rosso L, Insua C, Berardi V, Fornari MC, Brites F. Alterations in biomarkers of cardiovascular disease (CVD) in active acromegaly. Clinical endocrinology 2009; 70:88-95
- Boero L, Manavela M, Merono T, Maidana P, Gomez Rosso L, Brites F. GH levels and insulin sensitivity are differently associated with biomarkers of cardiovascular disease in active acromegaly. Clinical endocrinology2012; 77:579-585
- Arosio M, Sartore G, Rossi CM, Casati G, Faglia G, Manzato E. LDL physical properties, lipoprotein and Lp(a) levels in acromegalic patients. Effects of octreotide therapy. Italian Multicenter Octreotide Study Group. Atherosclerosis 2000; 151:551-557
- Beentjes JA, van Tol A, Sluiter WJ, Dullaart RP. Low plasma lecithin:cholesterol acyltransferase and lipid transfer protein activities in growth hormone deficient and acromegalic men: role in altered high density lipoproteins. Atherosclerosis 2000; 153:491-498
- Ciresi A, Amato MC, Pivonello R, Nazzari E, Grasso LF, Minuto F, Ferone D, Colao A, Giordano C. The metabolic profile in active acromegaly is gender-specific. The Journal of clinical endocrinology and metabolism2013; 98:E51-59
- Sesmilo G, Fairfield WP, Katznelson L, Pulaski K, Freda PU, Bonert V, Dimaraki E, Stavrou S, Vance ML, Hayden D, Klibanski A. Cardiovascular risk factors in acromegaly before and after normalization of serum IGF-I levels with the GH antagonist pegvisomant. J Clin Endocrinol Metab 2002; 87:1692-1699
- Parkinson C, Drake WM, Wieringa G, Yates AP, Besser GM, Trainer PJ. Serum lipoprotein changes following IGF-I normalization using a growth hormone receptor antagonist in acromegaly. Clin Endocrinol (Oxf) 2002; 56:303-311
- Maldonado Castro GF, Escobar-Morreale HF, Ortega H, Gomez-Coronado D, Balsa Barro JA, Varela C, Lasuncion MA. Effects of normalization of GH hypersecretion on lipoprotein(a) and other lipoprotein serum levels in acromegaly. Clinical endocrinology 2000; 53:313-319
- Berg C, Petersenn S, Lahner H, Herrmann BL, Buchfelder M, Droste M, Stalla GK, Strasburger CJ, Roggenbuck U, Lehmann N, Moebus S, Jockel KH, Mohlenkamp S, Erbel R, Saller B, Mann K, Investigative Group of the Heinz Nixdorf Recall S, the German Pegvisomant Observational Study B, Investigators. Cardiovascular risk factors in patients with uncontrolled and long-term acromegaly: comparison with matched data from the general population and the effect of disease control. The Journal of clinical endocrinology and metabolism 2010; 95:3648-3656
- Tan KC, Shiu SW, Janus ED, Lam KS. LDL subfractions in acromegaly: relation to growth hormone and insulin-like growth factor-I. Atherosclerosis 1997; 129:59-65
- Wildbrett J, Hanefeld M, Fucker K, Pinzer T, Bergmann S, Siegert G, Breidert M. Anomalies of lipoprotein pattern and fibrinolysis in acromegalic patients: relation to growth hormone levels and insulin-like growth factor I. Experimental and clinical endocrinology & diabetes : official journal, German Society of Endocrinology [and] German Diabetes Association 1997; 105:331-335
- Maffei P, Sicolo N, Plebani M. Lipoprotein(a) in acromegaly. Annals of internal medicine 1999; 130:537-538
- Lam KS, Pang RW, Janus ED, Kung AW, Wang CC. Serum apolipoprotein(a) correlates with growth hormone levels in Chinese patients with acromegaly. Atherosclerosis 1993; 104:183-188
- Tsuchiya H, Onishi T, Mogami H, Iida M. Lipid metabolism in acromegalic patients before and after selective pituitary adenomectomy. Endocrinologia japonica 1990; 37:797-807
- Tan KC, Pang RW, Tiu SC, Lam KS. Effects of treatment with Sandostatin LAR on small dense LDL and remnant-like lipoproteins in patients with acromegaly. Clinical endocrinology 2003; 59:558-564
- Reyes-Vidal C, Fernandez JC, Bruce JN, Crisman C, Conwell IM, Kostadinov J, Geer EB, Post KD, Freda PU. Prospective study of surgical treatment of acromegaly: effects on ghrelin, weight, adiposity, and markers of CV risk. The Journal of clinical endocrinology and metabolism 2014; 99:4124-4132
- Oscarsson J, Wiklund O, Jakobsson KE, Petruson B, Bengtsson BA. Serum lipoproteins in acromegaly before and 6-15 months after transsphenoidal adenomectomy. Clinical endocrinology 1994; 41:603-608
- James RA, Moller N, Chatterjee S, White M, Kendall-Taylor P. Carbohydrate tolerance and serum lipids in acromegaly before and during treatment with high dose octreotide. Diabetic medicine : a journal of the British Diabetic Association 1991; 8:517-523
- Cohen R, Chanson P, Bruckert E, Timsit J, Legrand A, Harris AG, Guillausseau PJ, Warnet A, Lubetzki J. Effects of octreotide on lipid metabolism in acromegaly. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme 1992; 24:397-400
- Cozzolino A, Feola T, Simonelli I, Puliani G, Hasenmajer V, Minnetti M, Giannetta E, Gianfrilli D, Pasqualetti P, Lenzi A, Isidori AM. Metabolic complications in acromegaly after neurosurgery: a meta-analysis. Eur J Endocrinol 2020; 183:597-606
- Muller AF, Leebeek FW, Janssen JA, Lamberts SW, Hofland L, van der Lely AJ. Acute effect of pegvisomant on cardiovascular risk markers in healthy men: implications for the pathogenesis of atherosclerosis in GH deficiency. J Clin Endocrinol Metab 2001; 86:5165-5171
- Murase T, Yamada N, Ohsawa N, Kosaka K, Morita S, Yoshida S. Decline of postheparin plasma lipoprotein lipase in acromegalic patients. Metabolism: clinical and experimental 1980; 29:666-672
- Twickler TB, Dallinga-Thie GM, Zelissen PM, Koppeschaar HP, Erkelens DW. The atherogenic plasma remnant-like particle cholesterol concentration is increased in the fasting and postprandial state in active acromegalic patients. Clinical endocrinology 2001; 55:69-75
- Feingold KR, Grunfeld C. Introduction to Lipids and Lipoproteins. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- Mosca S, Paolillo S, Colao A, Bossone E, Cittadini A, Iudice FL, Parente A, Conte S, Rengo G, Leosco D, Trimarco B, Filardi PP. Cardiovascular involvement in patients affected by acromegaly: an appraisal. International journal of cardiology 2013; 167:1712-1718
- Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocrine reviews 2004; 25:102-152
- Schofl C, Petroff D, Tonjes A, Grussendorf M, Droste M, Stalla G, Jaursch-Hancke C, Stormann S, Schopohl J. Incidence of myocardial infarction and stroke in acromegaly patients: results from the German Acromegaly Registry. Pituitary 2017; 20:635-642
- Hong S, Kim KS, Han K, Park CY. Acromegaly and cardiovascular outcomes: a cohort study. Eur Heart J 2022; 43:1491-1499
- Brevetti G, Marzullo P, Silvestro A, Pivonello R, Oliva G, di Somma C, Lombardi G, Colao A. Early vascular alterations in acromegaly. The Journal of clinical endocrinology and metabolism 2002; 87:3174-3179
- Colao A, Spiezia S, Cerbone G, Pivonello R, Marzullo P, Ferone D, Di Somma C, Assanti AP, Lombardi G. Increased arterial intima-media thickness by B-M mode echodoppler ultrasonography in acromegaly. Clinical endocrinology 2001; 54:515-524
- De Martino MC, Auriemma RS, Brevetti G, Vitale G, Schiano V, Galdiero M, Grasso L, Lombardi G, Colao A, Pivonello R. The treatment with growth hormone receptor antagonist in acromegaly: effect on vascular structure and function in patients resistant to somatostatin analogues. Journal of endocrinological investigation2010; 33:663-670
- Kartal I, Oflaz H, Pamukcu B, Meric M, Aral F, Ozbey N, Alagol F. Investigation of early atherosclerotic changes in acromegalic patients. International journal of clinical practice 2010; 64:39-44
- Ozkan C, Altinova AE, Cerit ET, Yayla C, Sahinarslan A, Sahin D, Dincel AS, Toruner FB, Akturk M, Arslan M. Markers of early atherosclerosis, oxidative stress and inflammation in patients with acromegaly. Pituitary 2015; 18:621-629
- Otsuki M, Kasayama S, Yamamoto H, Saito H, Sumitani S, Kouhara H, Saitoh Y, Ohnishi T, Arita N. Characterization of premature atherosclerosis of carotid arteries in acromegalic patients. Clinical endocrinology2001; 54:791-796
- Boysan SN, Kantarci F, Celik O, Mihmanli I, Gazioglu N, Kadioglu P. Atherosclerotic risk factors and premature atherosclerosis in acromegaly before and after 48 months of octreotide-LAR treatment. Angiology 2012; 63:522-527
- Akutsu H, Kreutzer J, Wasmeier G, Ropers D, Rost C, Mohlig M, Wallaschofski H, Buchfelder M, Schofl C. Acromegaly per se does not increase the risk for coronary artery disease. European journal of endocrinology / European Federation of Endocrine Societies 2010; 162:879-886
- Bogazzi F, Battolla L, Spinelli C, Rossi G, Gavioli S, Di Bello V, Cosci C, Sardella C, Volterrani D, Talini E, Pepe P, Falaschi F, Mariani G, Martino E. Risk factors for development of coronary heart disease in patients with acromegaly: a five-year prospective study. The Journal of clinical endocrinology and metabolism 2007; 92:4271-4277
- Cannavo S, Almoto B, Cavalli G, Squadrito S, Romanello G, Vigo MT, Fiumara F, Benvenga S, Trimarchi F. Acromegaly and coronary disease: an integrated evaluation of conventional coronary risk factors and coronary calcifications detected by computed tomography. The Journal of clinical endocrinology and metabolism 2006; 91:3766-3772
- Dos Santos Silva CM, Lima GA, Volschan IC, Gottlieb I, Kasuki L, Neto LV, Gadelha MR. Low risk of coronary artery disease in patients with acromegaly. Endocrine 2015; 50:749-755
- Herrmann BL, Severing M, Schmermund A, Berg C, Budde T, Erbel R, Mann K. Impact of disease duration on coronary calcification in patients with acromegaly. Experimental and clinical endocrinology & diabetes : official journal, German Society of Endocrinology [and] German Diabetes Association 2009; 117:417-422
- Duntas LH, Brenta G. The effect of thyroid disorders on lipid levels and metabolism. Med Clin North Am 2012; 96:269-281
- Retnakaran R, Connelly PW, Goguen J. Unmasking of type III hyperlipoproteinemia by hypothyroidism: a dramatic illustration of altered lipoprotein metabolism in a postpartum woman. Endocr Pract 2005; 11:394-398
- Feussner G, Ziegler R. Expression of type III hyperlipoproteinaemia in a subject with secondary hypothyroidism bearing the apolipoprotein E2/2 phenotype. J Intern Med 1991; 230:183-186
- Lindner MA, Illingworth DR. Expression of type III hyperlipoproteinemia in an adolescent patient with hypothyroidism. J Pediatr 1988; 113:86-89
- Verdugo C, Perrot L, Ponsin G, Valentin C, Berthezene F. Time-course of alterations of high density lipoproteins (HDL) during thyroxine administration to hypothyroid women. Eur J Clin Invest 1987; 17:313-316
- de Bruin TW, van Barlingen H, van Linde-Sibenius Trip M, van Vuurst de Vries AR, Akveld MJ, Erkelens DW. Lipoprotein(a) and apolipoprotein B plasma concentrations in hypothyroid, euthyroid, and hyperthyroid subjects. J Clin Endocrinol Metab 1993; 76:121-126
- Klausen IC, Nielsen FE, Hegedus L, Gerdes LU, Charles P, Faergeman O. Treatment of hypothyroidism reduces low-density lipoproteins but not lipoprotein(a). Metabolism 1992; 41:911-914
- Tzotzas T, Krassas GE, Konstantinidis T, Bougoulia M. Changes in lipoprotein(a) levels in overt and subclinical hypothyroidism before and during treatment. Thyroid 2000; 10:803-808
- Kaliaperumal R, William E, Selvam T, Krishnan SM. Relationship between Lipoprotein(a) and Thyroid Hormones in Hypothyroid Patients. J Clin Diagn Res 2014; 8:37-39
- Murase T, Arimoto S, Okubo M, Morinaga S. Significant reduction of elevated serum lipoprotein(a) concentrations during levo-thyroxine-replacement therapy in a hypothyroid patient. J Clin Lipidol 2012; 6:388-391
- O'Brien T, Dinneen SF, O'Brien PC, Palumbo PJ. Hyperlipidemia in patients with primary and secondary hypothyroidism. Mayo Clin Proc 1993; 68:860-866
- Valdemarsson S, Hedner P, Nilsson-Ehle P. Dyslipoproteinaemia in hypothyroidism of pituitary origin: effects of L-thyroxine substitution on lipoprotein lipase, hepatic lipase, and on plasma lipoproteins. Acta Endocrinol (Copenh) 1983; 103:192-197
- Ito M, Arishima T, Kudo T, Nishihara E, Ohye H, Kubota S, Fukata S, Amino N, Kuma K, Sasaki I, Hiraiwa T, Hanafusa T, Takamatsu J, Miyauchi A. Effect of levo-thyroxine replacement on non-high-density lipoprotein cholesterol in hypothyroid patients. J Clin Endocrinol Metab 2007; 92:608-611
- Jung KY, Ahn HY, Han SK, Park YJ, Cho BY, Moon MK. Association between thyroid function and lipid profiles, apolipoproteins, and high-density lipoprotein function. J Clin Lipidol 2017; 11:1347-1353
- Kotwal A, Cortes T, Genere N, Hamidi O, Jasim S, Newman CB, Prokop LJ, Murad MH, Alahdab F. Treatment of Thyroid Dysfunction and Serum Lipids: A Systematic Review and Meta-analysis. J Clin Endocrinol Metab2020; 105
- Pearce EN. Update in lipid alterations in subclinical hypothyroidism. J Clin Endocrinol Metab 2012; 97:326-333
- Wiersinga WM. Adult Hypothyroidism. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- Chubb SA, Davis WA, Davis TM. Interactions among thyroid function, insulin sensitivity, and serum lipid concentrations: the Fremantle diabetes study. J Clin Endocrinol Metab 2005; 90:5317-5320
- Rugge JB, Bougatsos C, Chou R. Screening and treatment of thyroid dysfunction: an evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162:35-45
- Meier C, Staub JJ, Roth CB, Guglielmetti M, Kunz M, Miserez AR, Drewe J, Huber P, Herzog R, Muller B. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical symptoms in subclinical hypothyroidism: a double blind, placebo-controlled trial (Basel Thyroid Study). J Clin Endocrinol Metab 2001; 86:4860-4866
- Ochs N, Auer R, Bauer DC, Nanchen D, Gussekloo J, Cornuz J, Rodondi N. Meta-analysis: subclinical thyroid dysfunction and the risk for coronary heart disease and mortality. Ann Intern Med 2008; 148:832-845
- Razvi S, Shakoor A, Vanderpump M, Weaver JU, Pearce SH. The influence of age on the relationship between subclinical hypothyroidism and ischemic heart disease: a metaanalysis. J Clin Endocrinol Metab2008; 93:2998-3007
- Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, Asvold BO, Iervasi G, Imaizumi M, Collet TH, Bremner A, Maisonneuve P, Sgarbi JA, Khaw KT, Vanderpump MP, Newman AB, Cornuz J, Franklyn JA, Westendorp RG, Vittinghoff E, Gussekloo J, Thyroid Studies C. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA 2010; 304:1365-1374
- Sun J, Yao L, Fang Y, Yang R, Chen Y, Yang K, Tian L. Relationship between Subclinical Thyroid Dysfunction and the Risk of Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Int J Endocrinol 2017; 2017:8130796
- Ning Y, Cheng YJ, Liu LJ, Sara JD, Cao ZY, Zheng WP, Zhang TS, Han HJ, Yang ZY, Zhang Y, Wang FL, Pan RY, Huang JL, Wu LL, Zhang M, Wei YX. What is the association of hypothyroidism with risks of cardiovascular events and mortality? A meta-analysis of 55 cohort studies involving 1,898,314 participants. BMC Med 2017; 15:21
- Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, Pessah-Pollack R, Singer PA, Woeber KA, American Association of Clinical E, American Thyroid Association Taskforce on Hypothyroidism in A. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract 2012; 18:988-1028
- Zhao T, Chen B, Zhou Y, Wang X, Zhang Y, Wang H, Shan Z. Effect of levothyroxine on the progression of carotid intima-media thickness in subclinical hypothyroidism patients: a meta-analysis. BMJ Open 2017; 7:e016053
- Aziz M, Kandimalla Y, Machavarapu A, Saxena A, Das S, Younus A, Nguyen M, Malik R, Anugula D, Latif MA, Humayun C, Khan IM, Adus A, Rasool A, Veledar E, Nasir K. Effect of Thyroxin Treatment on Carotid Intima-Media Thickness (CIMT) Reduction in Patients with Subclinical Hypothyroidism (SCH): a Meta-Analysis of Clinical Trials. J Atheroscler Thromb 2017; 24:643-659
- Gao N, Zhang W, Zhang YZ, Yang Q, Chen SH. Carotid intima-media thickness in patients with subclinical hypothyroidism: a meta-analysis. Atherosclerosis 2013; 227:18-25
- Blum MR, Gencer B, Adam L, Feller M, Collet TH, da Costa BR, Moutzouri E, Dopheide J, Depairon M, Sykiotis GP, Kearney P, Gussekloo J, Westendorp R, Stott DJ, Bauer DC, Rodondi N. Impact of Thyroid Hormone Therapy on Atherosclerosis in the Elderly With Subclinical Hypothyroidism: A Randomized Trial. J Clin Endocrinol Metab 2018; 103:2988-2997
- Park YJ, Lee YJ, Choi SI, Chun EJ, Jang HC, Chang HJ. Impact of subclinical hypothyroidism on the coronary artery disease in apparently healthy subjects. Eur J Endocrinol 2011; 165:115-121
- Silva N, Santos O, Morais F, Gottlieb I, Hadlich M, Rothstein T, Tauil M, Veras N, Vaisman M, Teixeira Pde F. Subclinical hypothyroidism represents an additional risk factor for coronary artery calcification, especially in subjects with intermediate and high cardiovascular risk scores. Eur J Endocrinol 2014; 171:327-334
- Verma R, Verma A, Gupta P, Agrawal NK. Coronary artery calcium scoring is a better predictor of cardiac risk in subclinical hypothyroidism patients with low-risk Framingham score. Indian J Endocrinol Metab 2016; 20:756-762
- Rosario PWS, Calsolari MR. Subclinical Hypothyroidism with TSH>7 mIU/l and</=10 mIU/l and Coronary Artery Disease. Horm Metab Res 2020; 52:85-88
- Walton KW, Scott PJ, Dykes PW, Davies JW. The significance of alterations in serum lipids in thyroid dysfunction. II. Alterations of the metabolism and turnover of 131-I-low-density lipoproteins in hypothyroidism and thyrotoxicosis. Clin Sci 1965; 29:217-238
- Chait A, Bierman EL, Albers JJ. Regulatory role of triiodothyronine in the degradation of low density lipoprotein by cultured human skin fibroblasts. J Clin Endocrinol Metab 1979; 48:887-889
- Staels B, Van Tol A, Chan L, Will H, Verhoeven G, Auwerx J. Alterations in thyroid status modulate apolipoprotein, hepatic triglyceride lipase, and low density lipoprotein receptor in rats. Endocrinology 1990; 127:1144-1152
- Salter AM, Hayashi R, al-Seeni M, Brown NF, Bruce J, Sorensen O, Atkinson EA, Middleton B, Bleackley RC, Brindley DN. Effects of hypothyroidism and high-fat feeding on mRNA concentrations for the low-density-lipoprotein receptor and on acyl-CoA:cholesterol acyltransferase activities in rat liver. Biochem J 1991; 276 ( Pt 3):825-832
- Scarabottolo L, Trezzi E, Roma P, Catapano AL. Experimental hypothyroidism modulates the expression of the low density lipoprotein receptor by the liver. Atherosclerosis 1986; 59:329-333
- Thompson GR, Soutar AK, Spengel FA, Jadhav A, Gavigan SJ, Myant NB. Defects of receptor-mediated low density lipoprotein catabolism in homozygous familial hypercholesterolemia and hypothyroidism in vivo. Proc Natl Acad Sci U S A 1981; 78:2591-2595
- Lopez D, Abisambra Socarras JF, Bedi M, Ness GC. Activation of the hepatic LDL receptor promoter by thyroid hormone. Biochim Biophys Acta 2007; 1771:1216-1225
- Shin DJ, Osborne TF. Thyroid hormone regulation and cholesterol metabolism are connected through Sterol Regulatory Element-Binding Protein-2 (SREBP-2). J Biol Chem 2003; 278:34114-34118
- Bonde Y, Breuer O, Lutjohann D, Sjoberg S, Angelin B, Rudling M. Thyroid hormone reduces PCSK9 and stimulates bile acid synthesis in humans. J Lipid Res 2014; 55:2408-2415
- Gong Y, Ma Y, Ye Z, Fu Z, Yang P, Gao B, Guo W, Hu D, Ye J, Ma S, Zhang F, Zhou L, Xu X, Li Z, Yang T, Zhou H. Thyroid stimulating hormone exhibits the impact on LDLR/LDL-c via up-regulating hepatic PCSK9 expression. Metabolism 2017; 76:32-41
- Goldberg IJ, Huang LS, Huggins LA, Yu S, Nagareddy PR, Scanlan TS, Ehrenkranz JR. Thyroid hormone reduces cholesterol via a non-LDL receptor-mediated pathway. Endocrinology 2012; 153:5143-5149
- Lin JZ, Martagon AJ, Hsueh WA, Baxter JD, Gustafsson JA, Webb P, Phillips KJ. Thyroid hormone receptor agonists reduce serum cholesterol independent of the LDL receptor. Endocrinology 2012; 153:6136-6144
- Day R, Gebhard RL, Schwartz HL, Strait KA, Duane WC, Stone BG, Oppenheimer JH. Time course of hepatic 3-hydroxy-3-methylglutaryl coenzyme A reductase activity and messenger ribonucleic acid, biliary lipid secretion, and hepatic cholesterol content in methimazole-treated hypothyroid and hypophysectomized rats after triiodothyronine administration: possible linkage of cholesterol synthesis to biliary secretion. Endocrinology 1989; 125:459-468
- Pandak WM, Heuman DM, Redford K, Stravitz RT, Chiang JY, Hylemon PB, Vlahcevic ZR. Hormonal regulation of cholesterol 7alpha-hydroxylase specific activity, mRNA levels, and transcriptional activity in vivo in the rat. J Lipid Res 1997; 38:2483-2491
- Ness GC, Pendleton LC, Li YC, Chiang JY. Effect of thyroid hormone on hepatic cholesterol 7 alpha hydroxylase, LDL receptor, HMG-CoA reductase, farnesyl pyrophosphate synthetase and apolipoprotein A-I mRNA levels in hypophysectomized rats. Biochem Biophys Res Commun 1990; 172:1150-1156
- Galman C, Bonde Y, Matasconi M, Angelin B, Rudling M. Dramatically increased intestinal absorption of cholesterol following hypophysectomy is normalized by thyroid hormone. Gastroenterology 2008; 134:1127-1136
- Tancevski I, Demetz E, Eller P, Duwensee K, Hoefer J, Heim C, Stanzl U, Wehinger A, Auer K, Karer R, Huber J, Schgoer W, Van Eck M, Vanhoutte J, Fievet C, Stellaard F, Rudling M, Patsch JR, Ritsch A. The liver-selective thyromimetic T-0681 influences reverse cholesterol transport and atherosclerosis development in mice. PLoS One 2010; 5:e8722
- Kuusi T, Taskinen MR, Nikkila EA. Lipoproteins, lipolytic enzymes, and hormonal status in hypothyroid women at different levels of substitution. J Clin Endocrinol Metab 1988; 66:51-56
- Abrams JJ, Grundy SM, Ginsberg H. Metabolism of plasma triglycerides in hypothyroidism and hyperthyroidism in man. J Lipid Res 1981; 22:307-322
- Lam KS, Chan MK, Yeung RT. High-density lipoprotein cholesterol, hepatic lipase and lipoprotein lipase activities in thyroid dysfunction--effects of treatment. Q J Med 1986; 59:513-521
- Lithell H, Boberg J, Hellsing K, Ljunghall S, Lundqvist G, Vessby B, Wide L. Serum lipoprotein and apolipoprotein concentrations and tissue lipoprotein-lipase activity in overt and subclinical hypothyroidism: the effect of substitution therapy. Eur J Clin Invest 1981; 11:3-10
- Dimitriadis G, Mitrou P, Lambadiari V, Boutati E, Maratou E, Panagiotakos DB, Koukkou E, Tzanela M, Thalassinos N, Raptis SA. Insulin action in adipose tissue and muscle in hypothyroidism. J Clin Endocrinol Metab 2006; 91:4930-4937
- Valdemarsson S, Hedner P, Nilsson-Ehle P. Reversal of decreased hepatic lipase and lipoprotein lipase activities after treatment of hypothyroidism. Eur J Clin Invest 1982; 12:423-428
- Prieur X, Huby T, Coste H, Schaap FG, Chapman MJ, Rodriguez JC. Thyroid hormone regulates the hypotriglyceridemic gene APOA5. J Biol Chem 2005; 280:27533-27543
- Fugier C, Tousaint JJ, Prieur X, Plateroti M, Samarut J, Delerive P. The lipoprotein lipase inhibitor ANGPTL3 is negatively regulated by thyroid hormone. J Biol Chem 2006; 281:11553-11559
- Yang L, Yin R, Wang Z, Wang X, Zhang Y, Zhao D. Circulating Angptl3 and Angptl8 Are Increased in Patients with Hypothyroidism. Biomed Res Int 2019; 2019:3814687
- Fabbrini E, Magkos F, Patterson BW, Mittendorfer B, Klein S. Subclinical hypothyroidism and hyperthyroidism have opposite effects on hepatic very-low-density lipoprotein-triglyceride kinetics. J Clin Endocrinol Metab2012; 97:E414-418
- Tan KC, Shiu SW, Kung AW. Plasma cholesteryl ester transfer protein activity in hyper- and hypothyroidism. J Clin Endocrinol Metab 1998; 83:140-143
- Tan KC, Shiu SW, Kung AW. Effect of thyroid dysfunction on high-density lipoprotein subfraction metabolism: roles of hepatic lipase and cholesteryl ester transfer protein. J Clin Endocrinol Metab 1998; 83:2921-2924
- Ridgway ND, Dolphin PJ. Serum activity and hepatic secretion of lecithin:cholesterol acyltransferase in experimental hypothyroidism and hypercholesterolemia. J Lipid Res 1985; 26:1300-1313
- Ritter MC, Kannan CR, Bagdade JD. The effects of hypothyroidism and replacement therapy on cholesteryl ester transfer. J Clin Endocrinol Metab 1996; 81:797-800
- Dullaart RP, Hoogenberg K, Groener JE, Dikkeschei LD, Erkelens DW, Doorenbos H. The activity of cholesteryl ester transfer protein is decreased in hypothyroidism: a possible contribution to alterations in high-density lipoproteins. Eur J Clin Invest 1990; 20:581-587
- Packard CJ, Shepherd J, Lindsay GM, Gaw A, Taskinen MR. Thyroid replacement therapy and its influence on postheparin plasma lipases and apolipoprotein-B metabolism in hypothyroidism. J Clin Endocrinol Metab 1993; 76:1209-1216
- Pazos F, Alvarez JJ, Rubies-Prat J, Varela C, Lasuncion MA. Long-term thyroid replacement therapy and levels of lipoprotein(a) and other lipoproteins. J Clin Endocrinol Metab 1995; 80:562-566
- Johansson L, Rudling M, Scanlan TS, Lundasen T, Webb P, Baxter J, Angelin B, Parini P. Selective thyroid receptor modulation by GC-1 reduces serum lipids and stimulates steps of reverse cholesterol transport in euthyroid mice. Proc Natl Acad Sci U S A 2005; 102:10297-10302
- Boone LR, Lagor WR, Moya Mde L, Niesen MI, Rothblat GH, Ness GC. Thyroid hormone enhances the ability of serum to accept cellular cholesterol via the ABCA1 transporter. Atherosclerosis 2011; 218:77-82
- Heimberg M, Olubadewo JO, Wilcox HG. Plasma lipoproteins and regulation of hepatic metabolism of fatty acids in altered thyroid states. Endocr Rev 1985; 6:590-607
- Russo L, Nguyen TNH, Kyrilli A, Robin M, Bel Lassen P, Moreno-Reyes R, Corvilain B. Metabolic Changes after Radioiodine Correction of Grade 1 and Grade 2 Subclinical Hyperthyroidism. Eur Thyroid J 2021; 10:382-389
- The coronary drug project. Findings leading to further modifications of its protocol with respect to dextrothyroxine. The coronary drug project research group. JAMA 1972; 220:996-1008
- Angelin B, Rudling M. Lipid lowering with thyroid hormone and thyromimetics. Curr Opin Lipidol 2010; 21:499-506
- Bonde Y, Plosch T, Kuipers F, Angelin B, Rudling M. Stimulation of murine biliary cholesterol secretion by thyroid hormone is dependent on a functional ABCG5/G8 complex. Hepatology 2012; 56:1828-1837
- Stein EA. Low-density lipoprotein cholesterol reduction by inhibition of PCSK9. Curr Opin Lipidol 2013; 24:510-517
- Arnaldi G, Scandali VM, Trementino L, Cardinaletti M, Appolloni G, Boscaro M. Pathophysiology of dyslipidemia in Cushing's syndrome. Neuroendocrinology 2010; 92 Suppl 1:86-90
- Arnaldi G, Angeli A, Atkinson AB, Bertagna X, Cavagnini F, Chrousos GP, Fava GA, Findling JW, Gaillard RC, Grossman AB, Kola B, Lacroix A, Mancini T, Mantero F, Newell-Price J, Nieman LK, Sonino N, Vance ML, Giustina A, Boscaro M. Diagnosis and complications of Cushing's syndrome: a consensus statement. J Clin Endocrinol Metab 2003; 88:5593-5602
- Mancini T, Kola B, Mantero F, Boscaro M, Arnaldi G. High cardiovascular risk in patients with Cushing's syndrome according to 1999 WHO/ISH guidelines. Clin Endocrinol (Oxf) 2004; 61:768-777
- Giordano R, Picu A, Marinazzo E, D'Angelo V, Berardelli R, Karamouzis I, Forno D, Zinna D, Maccario M, Ghigo E, Arvat E. Metabolic and cardiovascular outcomes in patients with Cushing's syndrome of different aetiologies during active disease and 1 year after remission. Clin Endocrinol (Oxf) 2011; 75:354-360
- Krsek M, Silha JV, Jezkova J, Hana V, Marek J, Weiss V, Stepan JJ, Murphy LJ. Adipokine levels in Cushing's syndrome; elevated resistin levels in female patients with Cushing's syndrome. Clin Endocrinol (Oxf) 2004; 60:350-357
- Faggiano A, Pivonello R, Spiezia S, De Martino MC, Filippella M, Di Somma C, Lombardi G, Colao A. Cardiovascular risk factors and common carotid artery caliber and stiffness in patients with Cushing's disease during active disease and 1 year after disease remission. J Clin Endocrinol Metab 2003; 88:2527-2533
- Colao A, Pivonello R, Spiezia S, Faggiano A, Ferone D, Filippella M, Marzullo P, Cerbone G, Siciliani M, Lombardi G. Persistence of increased cardiovascular risk in patients with Cushing's disease after five years of successful cure. J Clin Endocrinol Metab 1999; 84:2664-2672
- Li Z, Zhang C, Geng C, Song Y. Metabolic profile differences in ACTH-dependent and ACTH-independent Cushing syndrome. Chronic Dis Transl Med 2022; 8:36-40
- Feingold KR, Grunfeld C. Diabetes and Dyslipidemia. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- Taskinen MR, Nikkila EA, Pelkonen R, Sane T. Plasma lipoproteins, lipolytic enzymes, and very low density lipoprotein triglyceride turnover in Cushing's syndrome. J Clin Endocrinol Metab 1983; 57:619-626
- Friedman TC, Mastorakos G, Newman TD, Mullen NM, Horton EG, Costello R, Papadopoulos NM, Chrousos GP. Carbohydrate and lipid metabolism in endogenous hypercortisolism: shared features with metabolic syndrome X and NIDDM. Endocr J 1996; 43:645-655
- Ettinger WH, Jr., Hazzard WR. Prednisone increases very low density lipoprotein and high density lipoprotein in healthy men. Metabolism 1988; 37:1055-1058
- Zimmerman J, Fainaru M, Eisenberg S. The effects of prednisone therapy on plasma lipoproteins and apolipoproteins: a prospective study. Metabolism 1984; 33:521-526
- Taskinen MR, Kuusi T, Yki-Jarvinen H, Nikkila EA. Short-term effects of prednisone on serum lipids and high density lipoprotein subfractions in normolipidemic healthy men. J Clin Endocrinol Metab 1988; 67:291-299
- Feingold KR, Grunfeld C. The Effect of Inflammation and Infection on Lipids and Lipoproteins. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- de Guia RM, Herzig S. How Do Glucocorticoids Regulate Lipid Metabolism? Adv Exp Med Biol 2015; 872:127-144
- Macfarlane DP, Forbes S, Walker BR. Glucocorticoids and fatty acid metabolism in humans: fuelling fat redistribution in the metabolic syndrome. J Endocrinol 2008; 197:189-204
- Hazra A, Pyszczynski NA, DuBois DC, Almon RR, Jusko WJ. Modeling of corticosteroid effects on hepatic low-density lipoprotein receptors and plasma lipid dynamics in rats. Pharm Res 2008; 25:769-780
- Galman C, Angelin B, Rudling M. Prolonged stimulation of the adrenals by corticotropin suppresses hepatic low-density lipoprotein and high-density lipoprotein receptors and increases plasma cholesterol. Endocrinology2002; 143:1809-1816
- Amatruda JM, Danahy SA, Chang CL. The effects of glucocorticoids on insulin-stimulated lipogenesis in primary cultures of rat hepatocytes. Biochem J 1983; 212:135-141
- Diamant S, Shafrir E. Modulation of the activity of insulin-dependent enzymes of lipogenesis by glucocorticoids. Eur J Biochem 1975; 53:541-546
- Krausz Y, Bar-On H, Shafrir E. Origin and pattern of glucocorticoid-induced hyperlipidemia in rats. Dose-dependent bimodal changes in serum lipids and lipoproteins in relation to hepatic lipogenesis and tissue lipoprotein lipase activity. Biochim Biophys Acta 1981; 663:69-82
- Mangiapane EH, Brindley DN. Effects of dexamethasone and insulin on the synthesis of triacylglycerols and phosphatidylcholine and the secretion of very-low-density lipoproteins and lysophosphatidylcholine by monolayer cultures of rat hepatocytes. Biochem J 1986; 233:151-160
- Lau DC, Roncari DA. Effects of glucocorticoid hormones on lipid-synthetic enzymes from different adipose tissue regions and from liver. Can J Biochem Cell Biol 1983; 61:1245-1250
- Pittner RA, Fears R, Brindley DN. Interactions of insulin, glucagon and dexamethasone in controlling the activity of glycerol phosphate acyltransferase and the activity and subcellular distribution of phosphatidate phosphohydrolase in cultured rat hepatocytes. Biochem J 1985; 230:525-534
- Dolinsky VW, Douglas DN, Lehner R, Vance DE. Regulation of the enzymes of hepatic microsomal triacylglycerol lipolysis and re-esterification by the glucocorticoid dexamethasone. Biochem J 2004; 378:967-974
- Wang CN, McLeod RS, Yao Z, Brindley DN. Effects of dexamethasone on the synthesis, degradation, and secretion of apolipoprotein B in cultured rat hepatocytes. Arterioscler Thromb Vasc Biol 1995; 15:1481-1491
- Cole TG, Wilcox HG, Heimberg M. Effects of adrenalectomy and dexamethasone on hepatic lipid metabolism. J Lipid Res 1982; 23:81-91
- Martin-Sanz P, Vance JE, Brindley DN. Stimulation of apolipoprotein secretion in very-low-density and high-density lipoproteins from cultured rat hepatocytes by dexamethasone. Biochem J 1990; 271:575-583
- Peckett AJ, Wright DC, Riddell MC. The effects of glucocorticoids on adipose tissue lipid metabolism. Metabolism 2011; 60:1500-1510
- Campbell JE, Peckett AJ, D'Souza A M, Hawke TJ, Riddell MC. Adipogenic and lipolytic effects of chronic glucocorticoid exposure. Am J Physiol Cell Physiol 2011; 300:C198-209
- Fain JN, Kovacev VP, Scow RO. Effect of growth hormone and dexamethasone on lipolysis and metabolism in isolated fat cells of the rat. J Biol Chem 1965; 240:3522-3529
- Samra JS, Clark ML, Humphreys SM, MacDonald IA, Bannister PA, Frayn KN. Effects of physiological hypercortisolemia on the regulation of lipolysis in subcutaneous adipose tissue. J Clin Endocrinol Metab 1998; 83:626-631
- Xu C, He J, Jiang H, Zu L, Zhai W, Pu S, Xu G. Direct effect of glucocorticoids on lipolysis in adipocytes. Mol Endocrinol 2009; 23:1161-1170
- Djurhuus CB, Gravholt CH, Nielsen S, Mengel A, Christiansen JS, Schmitz OE, Moller N. Effects of cortisol on lipolysis and regional interstitial glycerol levels in humans. Am J Physiol Endocrinol Metab 2002; 283:E172-177
- Divertie GD, Jensen MD, Miles JM. Stimulation of lipolysis in humans by physiological hypercortisolemia. Diabetes 1991; 40:1228-1232
- Slavin BG, Ong JM, Kern PA. Hormonal regulation of hormone-sensitive lipase activity and mRNA levels in isolated rat adipocytes. J Lipid Res 1994; 35:1535-1541
- Villena JA, Roy S, Sarkadi-Nagy E, Kim KH, Sul HS. Desnutrin, an adipocyte gene encoding a novel patatin domain-containing protein, is induced by fasting and glucocorticoids: ectopic expression of desnutrin increases triglyceride hydrolysis. J Biol Chem 2004; 279:47066-47075
- Birkenhager JC, Timmermans HA, Lamberts SW. Depressed plasma FFA turnover rate in Cushing's syndrome. J Clin Endocrinol Metab 1976; 42:28-32
- Saunders J, Hall SE, Sonksen PH. Glucose and free fatty acid turnover in Cushing's syndrome. J Endocrinol Invest 1980; 3:309-311
- Saladin R, Vu-Dac N, Fruchart JC, Auwerx J, Staels B. Transcriptional induction of rat liver apolipoprotein A-I gene expression by glucocorticoids requires the glucocorticoid receptor and a labile cell-specific protein. Eur J Biochem 1996; 239:451-459
- Taylor AH, Raymond J, Dionne JM, Romney J, Chan J, Lawless DE, Wanke IE, Wong NC. Glucocorticoid increases rat apolipoprotein A-I promoter activity. J Lipid Res 1996; 37:2232-2243
- Jansen H, van Tol A, Auwerx J, Skretting G, Staels B. Opposite regulation of hepatic lipase and lecithin: cholesterol acyltransferase by glucocorticoids in rats. Biochim Biophys Acta 1992; 1128:181-185
- Etxabe J, Vazquez JA. Morbidity and mortality in Cushing's disease: an epidemiological approach. Clin Endocrinol (Oxf) 1994; 40:479-484
- Graversen D, Vestergaard P, Stochholm K, Gravholt CH, Jorgensen JO. Mortality in Cushing's syndrome: a systematic review and meta-analysis. Eur J Intern Med 2012; 23:278-282
- Ntali G, Asimakopoulou A, Siamatras T, Komninos J, Vassiliadi D, Tzanela M, Tsagarakis S, Grossman AB, Wass JA, Karavitaki N. Mortality in Cushing's syndrome: systematic analysis of a large series with prolonged follow-up. Eur J Endocrinol 2013; 169:715-723
- Clayton RN, Jones PW, Reulen RC, Stewart PM, Hassan-Smith ZK, Ntali G, Karavitaki N, Dekkers OM, Pereira AM, Bolland M, Holdaway I, Lindholm J. Mortality in patients with Cushing's disease more than 10 years after remission: a multicentre, multinational, retrospective cohort study. Lancet Diabetes Endocrinol2016; 4:569-576
- van Haalen FM, Broersen LH, Jorgensen JO, Pereira AM, Dekkers OM. Management of endocrine disease: Mortality remains increased in Cushing's disease despite biochemical remission: a systematic review and meta-analysis. Eur J Endocrinol 2015; 172:R143-149
- Dekkers OM, Horvath-Puho E, Jorgensen JO, Cannegieter SC, Ehrenstein V, Vandenbroucke JP, Pereira AM, Sorensen HT. Multisystem morbidity and mortality in Cushing's syndrome: a cohort study. J Clin Endocrinol Metab 2013; 98:2277-2284
- Albiger N, Testa RM, Almoto B, Ferrari M, Bilora F, Petrobelli F, Pagnan A, Mantero F, Scaroni C. Patients with Cushing's syndrome have increased intimal media thickness at different vascular levels: comparison with a population matched for similar cardiovascular risk factors. Horm Metab Res 2006; 38:405-410
- Bassareo PP, Fanos V, Zaffanello M, Mercuro G. Early markers of cardiovascular dysfunction in young girls affected by Cushing's syndrome before and after successful cure. J Pediatr Endocrinol Metab 2010; 23:627-635
- Petramala L, Lorenzo D, Iannucci G, Concistre A, Zinnamosca L, Marinelli C, De Vincentis G, Ciardi A, De Toma G, Letizia C. Subclinical Atherosclerosis in Patients with Cushing Syndrome: Evaluation with Carotid Intima-Media Thickness and Ankle-Brachial Index. Endocrinol Metab (Seoul) 2015; 30:488-493
- Barahona MJ, Resmini E, Vilades D, Pons-Llado G, Leta R, Puig T, Webb SM. Coronary artery disease detected by multislice computed tomography in patients after long-term cure of Cushing's syndrome. J Clin Endocrinol Metab 2013; 98:1093-1099
- Neary NM, Booker OJ, Abel BS, Matta JR, Muldoon N, Sinaii N, Pettigrew RI, Nieman LK, Gharib AM. Hypercortisolism is associated with increased coronary arterial atherosclerosis: analysis of noninvasive coronary angiography using multidetector computerized tomography. J Clin Endocrinol Metab 2013; 98:2045-2052
- Fardet L, Petersen I, Nazareth I. Risk of cardiovascular events in people prescribed glucocorticoids with iatrogenic Cushing's syndrome: cohort study. BMJ 2012; 345:e4928
- Souverein PC, Berard A, Van Staa TP, Cooper C, Egberts AC, Leufkens HG, Walker BR. Use of oral glucocorticoids and risk of cardiovascular and cerebrovascular disease in a population based case-control study. Heart 2004; 90:859-865
- Wei L, MacDonald TM, Walker BR. Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med 2004; 141:764-770
- Varas-Lorenzo C, Rodriguez LA, Maguire A, Castellsague J, Perez-Gutthann S. Use of oral corticosteroids and the risk of acute myocardial infarction. Atherosclerosis 2007; 192:376-383
- Sharma ST, Nieman LK, Feelders RA. Comorbidities in Cushing's disease. Pituitary 2015; 18:188-194
- De Leo M, Pivonello R, Auriemma RS, Cozzolino A, Vitale P, Simeoli C, De Martino MC, Lombardi G, Colao A. Cardiovascular disease in Cushing's syndrome: heart versus vasculature. Neuroendocrinology 2010; 92 Suppl 1:50-54
- Newman CB, Blaha MJ, Boord JB, Cariou B, Chait A, Fein HG, Ginsberg HN, Goldberg IJ, Murad MH, Subramanian S, Tannock LR. Lipid Management in Patients with Endocrine Disorders: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2020; 105
- Gylling H, Vanhanen H, Miettinen TA. Effects of ketoconazole on cholesterol precursors and low density lipoprotein kinetics in hypercholesterolemia. J Lipid Res 1993; 34:59-67
- Miettinen TA. Cholesterol metabolism during ketoconazole treatment in man. J Lipid Res 1988; 29:43-51
- Gylling H, Vanhanen H, Miettinen TA. Hypolipidemic effect and mechanism of ketoconazole without and with cholestyramine in familial hypercholesterolemia. Metabolism 1991; 40:35-41
- Fleseriu M, Auchus RJ, Greenman Y, Zacharieva S, Geer EB, Salvatori R, Pivonello R, Feldt-Rasmussen U, Kennedy L, Buchfelder M, Biller BM, Cohen F, Heaney AP. Levoketoconazole treatment in endogenous Cushing's syndrome: extended evaluation of clinical, biochemical, and radiologic outcomes. Eur J Endocrinol2022; 187:859-871
- Feingold KR GC. Cholesterol Lowering Drugs. In: De Groot LJ B-PP, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, ed.
. South Dartmouth (MA: MDText.com, Inc; 2016.
- Maher VM, Trainer PJ, Scoppola A, Anderson JV, Thompson GR, Besser GM. Possible mechanism and treatment of o,p'DDD-induced hypercholesterolaemia. Q J Med 1992; 84:671-679
- Shawa H, Deniz F, Bazerbashi H, Hernandez M, Vassilopoulou-Sellin R, Jimenez C, Habra MA. Mitotane-induced hyperlipidemia: a retrospective cohort study. Int J Endocrinol 2013; 2013:624962
- Bianchini M, Puliani G, Chiefari A, Mormando M, Lauretta R, Appetecchia M. Metabolic and Endocrine Toxicities of Mitotane: A Systematic Review. Cancers (Basel) 2021; 13
- Stacpoole PW, Varnado CE, Island DP. Stimulation of rat liver 3-hydroxy-3-methylglutaryl-coenzyme A reductase activity by o,p'-DDD. Biochem Pharmacol 1982; 31:857-860
- Tada H, Nohara A, Kawashiri MA, Inazu A, Mabuchi H, Yamagishi M. Marked transient hypercholesterolemia caused by low-dose mitotane as adjuvant chemotherapy for adrenocortical carcinoma. J Atheroscler Thromb2014; 21:1326-1329
- Page ST, Krauss RM, Gross C, Ishida B, Heinecke JW, Tang C, Amory JK, Schaefer PM, Cox CJ, Kane J, Purnell JQ, Weinstein RL, Vaisar T. Impact of mifepristone, a glucocorticoid/progesterone antagonist, on HDL cholesterol, HDL particle concentration, and HDL function. J Clin Endocrinol Metab 2012; 97:1598-1605
- Ottosson M, Marin P, Karason K, Elander A, Bjorntorp P. Blockade of the glucocorticoid receptor with RU 486: effects in vitro and in vivo on human adipose tissue lipoprotein lipase activity. Obes Res 1995; 3:233-240
- Pivonello R, Arnaldi G, Scaroni C, Giordano C, Cannavo S, Iacuaniello D, Trementino L, Zilio M, Guarnotta V, Albani A, Cozzolino A, Michetti G, Boscaro M, Colao A. The medical treatment with pasireotide in Cushing's disease: an Italian multicentre experience based on "real-world evidence". Endocrine 2019; 64:657-672
- Albani A, Ferrau F, Ciresi A, Pivonello R, Scaroni C, Iacuaniello D, Zilio M, Guarnotta V, Alibrandi A, Messina E, Boscaro M, Giordano C, Colao A, Cannavo S. Pasireotide treatment reduces cardiometabolic risk in Cushing's disease patients: an Italian, multicenter study. Endocrine 2018; 61:118-124
- Pivonello R, Petersenn S, Newell-Price J, Findling JW, Gu F, Maldonado M, Trovato A, Hughes G, Salgado LR, Lacroix A, Schopohl J, Biller BM, Pasireotide BSG. Pasireotide treatment significantly improves clinical signs and symptoms in patients with Cushing's disease: results from a Phase III study. Clin Endocrinol (Oxf)2014; 81:408-417
- Agledahl I, Skjaerpe PA, Hansen JB, Svartberg J. Low serum testosterone in men is inversely associated with non-fasting serum triglycerides: the Tromso study. Nutr Metab Cardiovasc Dis 2008; 18:256-262
- Haffner SM, Mykkanen L, Valdez RA, Katz MS. Relationship of sex hormones to lipids and lipoproteins in nondiabetic men. J Clin Endocrinol Metab 1993; 77:1610-1615
- Khaw KT, Barrett-Connor E. Endogenous sex hormones, high density lipoprotein cholesterol, and other lipoprotein fractions in men. Arterioscler Thromb 1991; 11:489-494
- Makinen JI, Perheentupa A, Irjala K, Pollanen P, Makinen J, Huhtaniemi I, Raitakari OT. Endogenous testosterone and serum lipids in middle-aged men. Atherosclerosis 2008; 197:688-693
- Van Pottelbergh I, Braeckman L, De Bacquer D, De Backer G, Kaufman JM. Differential contribution of testosterone and estradiol in the determination of cholesterol and lipoprotein profile in healthy middle-aged men. Atherosclerosis 2003; 166:95-102
- Hamalainen E, Adlercreutz H, Ehnholm C, Puska P. Relationships of serum lipoproteins and apoproteins to sex hormones and to the binding capacity of sex hormone binding globulin in healthy Finnish men. Metabolism1986; 35:535-541
- Wu FC, von Eckardstein A. Androgens and coronary artery disease. Endocr Rev 2003; 24:183-217
- Gyllenborg J, Rasmussen SL, Borch-Johnsen K, Heitmann BL, Skakkebaek NE, Juul A. Cardiovascular risk factors in men: The role of gonadal steroids and sex hormone-binding globulin. Metabolism 2001; 50:882-888
- Brand JS, van der Tweel I, Grobbee DE, Emmelot-Vonk MH, van der Schouw YT. Testosterone, sex hormone-binding globulin and the metabolic syndrome: a systematic review and meta-analysis of observational studies. Int J Epidemiol 2011; 40:189-207
- Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, Lenzi A, Forti G, Mannucci E, Maggi M. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med 2011; 8:272-283
- Bann D, Wu FC, Keevil B, Lashen H, Adams J, Hardy R, Muniz G, Kuh D, Ben-Shlomo Y, Ong KK. Changes in testosterone related to body composition in late midlife: Findings from the 1946 British birth cohort study. Obesity (Silver Spring) 2015; 23:1486-1492
- Corona G, Monami M, Rastrelli G, Aversa A, Sforza A, Lenzi A, Forti G, Mannucci E, Maggi M. Type 2 diabetes mellitus and testosterone: a meta-analysis study. Int J Androl 2011; 34:528-540
- Corona G, Rastrelli G, Monami M, Saad F, Luconi M, Lucchese M, Facchiano E, Sforza A, Forti G, Mannucci E, Maggi M. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. Eur J Endocrinol 2013; 168:829-843
- Sarwer DB, Spitzer JC, Wadden TA, Rosen RC, Mitchell JE, Lancaster K, Courcoulas A, Gourash W, Christian NJ. Sexual functioning and sex hormones in men who underwent bariatric surgery. Surg Obes Relat Dis 2015; 11:643-651
- Behre HM, Bockers A, Schlingheider A, Nieschlag E. Sustained suppression of serum LH, FSH and testosterone and increase of high-density lipoprotein cholesterol by daily injections of the GnRH antagonist cetrorelix over 8 days in normal men. Clin Endocrinol (Oxf) 1994; 40:241-248
- Mohamedali HZ, Breunis H, Timilshina N, Alibhai SM. Changes in blood glucose and cholesterol levels due to androgen deprivation therapy in men with non-metastatic prostate cancer. Can Urol Assoc J 2011; 5:28-32
- Saglam HS, Kose O, Kumsar S, Budak S, Adsan O. Fasting blood glucose and lipid profile alterations following twelve-month androgen deprivation therapy in men with prostate cancer. ScientificWorldJournal 2012; 2012:696329
- Smith MR, Finkelstein JS, McGovern FJ, Zietman AL, Fallon MA, Schoenfeld DA, Kantoff PW. Changes in body composition during androgen deprivation therapy for prostate cancer. J Clin Endocrinol Metab 2002; 87:599-603
- Eri LM, Urdal P, Bechensteen AG. Effects of the luteinizing hormone-releasing hormone agonist leuprolide on lipoproteins, fibrinogen and plasminogen activator inhibitor in patients with benign prostatic hyperplasia. J Urol1995; 154:100-104
- Bagatell CJ, Knopp RH, Vale WW, Rivier JE, Bremner WJ. Physiologic testosterone levels in normal men suppress high-density lipoprotein cholesterol levels. Ann Intern Med 1992; 116:967-973
- Yannucci J, Manola J, Garnick MB, Bhat G, Bubley GJ. The effect of androgen deprivation therapy on fasting serum lipid and glucose parameters. J Urol 2006; 176:520-525
- von Eckardstein A, Kliesch S, Nieschlag E, Chirazi A, Assmann G, Behre HM. Suppression of endogenous testosterone in young men increases serum levels of high density lipoprotein subclass lipoprotein A-I and lipoprotein(a). J Clin Endocrinol Metab 1997; 82:3367-3372
- Braga-Basaria M, Muller DC, Carducci MA, Dobs AS, Basaria S. Lipoprotein profile in men with prostate cancer undergoing androgen deprivation therapy. Int J Impot Res 2006; 18:494-498
- Torimoto K, Samma S, Kagebayashi Y, Chihara Y, Tanaka N, Hirayama A, Fujimoto K, Hirao Y. The effects of androgen deprivation therapy on lipid metabolism and body composition in Japanese patients with prostate cancer. Jpn J Clin Oncol 2011; 41:577-581
- Salvador C, Planas J, Agreda F, Placer J, Trilla E, Lopez MA, Morote J. Analysis of the lipid profile and atherogenic risk during androgen deprivation therapy in prostate cancer patients. Urol Int 2013; 90:41-44
- Cakici MC, Can B, Kazan O, Efiloglu O, Sendogan F, Ucar T, Turan T, Yildirim A. Effects of androgen deprivation therapy on metabolic markers and bioelectrical impedance analyze in prostate cancer patients. Rev Int Androl 2022; 20:96-101
- Whitsel EA, Boyko EJ, Matsumoto AM, Anawalt BD, Siscovick DS. Intramuscular testosterone esters and plasma lipids in hypogonadal men: a meta-analysis. Am J Med 2001; 111:261-269
- Isidori AM, Giannetta E, Greco EA, Gianfrilli D, Bonifacio V, Isidori A, Lenzi A, Fabbri A. Effects of testosterone on body composition, bone metabolism and serum lipid profile in middle-aged men: a meta-analysis. Clin Endocrinol (Oxf) 2005; 63:280-293
- Fernandez-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, Agrwal N, Elamin MB, Gallegos-Orozco JF, Wang AT, Erwin PJ, Bhasin S, Montori VM. Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab 2010; 95:2560-2575
- Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Bolona ER, Sideras K, Uraga MV, Erwin PJ, Montori VM. Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 2007; 82:29-39
- Corona G, Giagulli VA, Maseroli E, Vignozzi L, Aversa A, Zitzmann M, Saad F, Mannucci E, Maggi M. THERAPY OF ENDOCRINE DISEASE: Testosterone supplementation and body composition: results from a meta-analysis study. Eur J Endocrinol 2016; 174:R99-116
- Kumari K, Kumar R, Memon A, Kumari B, Tehrim M, Kumari P, Shehryar M, Islam H, Islam R, Khatri M, Kumar S, Kumar A. Treatment with Testosterone Therapy in Type 2 Diabetic Hypogonadal Adult Males: A Systematic Review and Meta-Analysis. Clin Pract 2023; 13:454-469
- Yassin A, Haider A, Haider KS, Caliber M, Doros G, Saad F, Garvey WT. Testosterone Therapy in Men With Hypogonadism Prevents Progression From Prediabetes to Type 2 Diabetes: Eight-Year Data From a Registry Study. Diabetes Care 2019; 42:1104-1111
- Schleich F, Legros JJ. Effects of androgen substitution on lipid profile in the adult and aging hypogonadal male. Eur J Endocrinol 2004; 151:415-424
- Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl2008; 29:102-105
- Anderson RA, Wallace EM, Wu FC. Effect of testosterone enanthate on serum lipoproteins in man. Contraception 1995; 52:115-119
- Friedl KE, Hannan CJ, Jr., Jones RE, Plymate SR. High-density lipoprotein cholesterol is not decreased if an aromatizable androgen is administered. Metabolism 1990; 39:69-74
- Thompson PD, Cullinane EM, Sady SP, Chenevert C, Saritelli AL, Sady MA, Herbert PN. Contrasting effects of testosterone and stanozolol on serum lipoprotein levels. JAMA 1989; 261:1165-1168
- Mohler ER, 3rd, Ellenberg SS, Lewis CE, Wenger NK, Budoff MJ, Lewis MR, Barrett-Connor E, Swerdloff RS, Stephens-Shields A, Bhasin S, Cauley JA, Crandall JP, Cunningham GR, Ensrud KE, Gill TM, Matsumoto AM, Molitch ME, Pahor M, Preston PE, Hou X, Cifelli D, Snyder PJ. The Effect of Testosterone on Cardiovascular Biomarkers in the Testosterone Trials. J Clin Endocrinol Metab 2018; 103:681-688
- Webb OL, Laskarzewski PM, Glueck CJ. Severe depression of high-density lipoprotein cholesterol levels in weight lifters and body builders by self-administered exogenous testosterone and anabolic-androgenic steroids. Metabolism 1984; 33:971-975
- Hurley BF, Seals DR, Hagberg JM, Goldberg AC, Ostrove SM, Holloszy JO, Wiest WG, Goldberg AP. High-density-lipoprotein cholesterol in bodybuilders v powerlifters. Negative effects of androgen use. JAMA 1984; 252:507-513
- Kuipers H, Wijnen JA, Hartgens F, Willems SM. Influence of anabolic steroids on body composition, blood pressure, lipid profile and liver functions in body builders. Int J Sports Med 1991; 12:413-418
- Vermeulen A, Kaufman JM, Goemaere S, van Pottelberg I. Estradiol in elderly men. Aging Male 2002; 5:98-102
- van Velzen DM, Paldino A, Klaver M, Nota NM, Defreyne J, Hovingh GK, Thijs A, Simsek S, T'Sjoen G, den Heijer M. Cardiometabolic Effects of Testosterone in Transmen and Estrogen Plus Cyproterone Acetate in Transwomen. J Clin Endocrinol Metab 2019; 104:1937-1947
- Gava G, Mancini I, Cerpolini S, Baldassarre M, Seracchioli R, Meriggiola MC. Testosterone undecanoate and testosterone enanthate injections are both effective and safe in transmen over 5 years of administration. Clin Endocrinol (Oxf) 2018; 89:878-886
- Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, Davidge-Pitts CJ, Nippoldt TB, Prokop LJ, Murad MH. Sex Steroids and Cardiovascular Outcomes in Transgender Individuals: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab 2017; 102:3914-3923
- Leemaqz SY, Kyinn M, Banks K, Sarkodie E, Goldstein D, Irwig MS. Lipid profiles and hypertriglyceridemia among transgender and gender diverse adults on gender-affirming hormone therapy. J Clin Lipidol 2023; 17:103-111
- Allen AN, Jiao R, Day P, Pagels P, Gimpel N, SoRelle JA. Dynamic Impact of Hormone Therapy on Laboratory Values in Transgender Patients over Time. J Appl Lab Med 2021; 6:27-40
- Millington K, Chan YM. Lipoprotein subtypes after testosterone therapy in transmasculine adolescents. J Clin Lipidol 2021; 15:840-844
- Kaplan SA, Lin J, Johnson-Levonas AO, Shah AK, Meehan AG. Increased occurrence of marked elevations of lipoprotein(a) in ageing, hypercholesterolaemic men with low testosterone. Aging Male 2010; 13:40-43
- Henriksson P, Angelin B, Berglund L. Hormonal regulation of serum Lp (a) levels. Opposite effects after estrogen treatment and orchidectomy in males with prostatic carcinoma. J Clin Invest 1992; 89:1166-1171
- Zmunda JM, Thompson PD, Dickenson R, Bausserman LL. Testosterone decreases lipoprotein(a) in men. Am J Cardiol 1996; 77:1244-1247
- Marcovina SM, Lippi G, Bagatell CJ, Bremner WJ. Testosterone-induced suppression of lipoprotein(a) in normal men; relation to basal lipoprotein(a) level. Atherosclerosis 1996; 122:89-95
- Glazer G. Atherogenic effects of anabolic steroids on serum lipid levels. A literature review. Arch Intern Med1991; 151:1925-1933
- Langer C, Gansz B, Goepfert C, Engel T, Uehara Y, von Dehn G, Jansen H, Assmann G, von Eckardstein A. Testosterone up-regulates scavenger receptor BI and stimulates cholesterol efflux from macrophages. Biochem Biophys Res Commun 2002; 296:1051-1057
- Tan KC, Shiu SW, Kung AW. Alterations in hepatic lipase and lipoprotein subfractions with transdermal testosterone replacement therapy. Clin Endocrinol (Oxf) 1999; 51:765-769
- Zmuda JM, Fahrenbach MC, Younkin BT, Bausserman LL, Terry RB, Catlin DH, Thompson PD. The effect of testosterone aromatization on high-density lipoprotein cholesterol level and postheparin lipolytic activity. Metabolism 1993; 42:446-450
- Sorva R, Kuusi T, Taskinen MR, Perheentupa J, Nikkila EA. Testosterone substitution increases the activity of lipoprotein lipase and hepatic lipase in hypogonadal males. Atherosclerosis 1988; 69:191-197
- Haffner SM, Kushwaha RS, Foster DM, Applebaum-Bowden D, Hazzard WR. Studies on the metabolic mechanism of reduced high density lipoproteins during anabolic steroid therapy. Metabolism 1983; 32:413-420
- Croston GE, Milan LB, Marschke KB, Reichman M, Briggs MR. Androgen receptor-mediated antagonism of estrogen-dependent low density lipoprotein receptor transcription in cultured hepatocytes. Endocrinology 1997; 138:3779-3786
- Yeap BB, Dwivedi G. Androgens and Cardiovascular Disease in Men. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrere B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, eds. Endotext. South Dartmouth (MA)2022.
- Zhao J, Zhu S, Sun L, Meng F, Zhao L, Zhao Y, Tian H, Li P, Niu Y. Androgen deprivation therapy for prostate cancer is associated with cardiovascular morbidity and mortality: a meta-analysis of population-based observational studies. PLoS One 2014; 9:e107516
- Carneiro A, Sasse AD, Wagner AA, Peixoto G, Kataguiri A, Neto AS, Bianco BA, Chang P, Pompeo AC, Tobias-Machado M. Cardiovascular events associated with androgen deprivation therapy in patients with prostate cancer: a systematic review and meta-analysis. World J Urol 2015; 33:1281-1289
- Nguyen PL, Je Y, Schutz FA, Hoffman KE, Hu JC, Parekh A, Beckman JA, Choueiri TK. Association of androgen deprivation therapy with cardiovascular death in patients with prostate cancer: a meta-analysis of randomized trials. JAMA 2011; 306:2359-2366
- Bosco C, Bosnyak Z, Malmberg A, Adolfsson J, Keating NL, Van Hemelrijck M. Quantifying observational evidence for risk of fatal and nonfatal cardiovascular disease following androgen deprivation therapy for prostate cancer: a meta-analysis. Eur Urol 2015; 68:386-396
- Layton JB, Meier CR, Sharpless JL, Sturmer T, Jick SS, Brookhart MA. Comparative Safety of Testosterone Dosage Forms. JAMA Intern Med 2015; 175:1187-1196
- Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, Eder R, Tennstedt S, Ulloor J, Zhang A, Choong K, Lakshman KM, Mazer NA, Miciek R, Krasnoff J, Elmi A, Knapp PE, Brooks B, Appleman E, Aggarwal S, Bhasin G, Hede-Brierley L, Bhatia A, Collins L, LeBrasseur N, Fiore LD, Bhasin S. Adverse events associated with testosterone administration. N Engl J Med 2010; 363:109-122
- Srinivas-Shankar U, Roberts SA, Connolly MJ, O'Connell MD, Adams JE, Oldham JA, Wu FC. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab 2010; 95:639-650
- Basaria S, Harman SM, Travison TG, Hodis H, Tsitouras P, Budoff M, Pencina KM, Vita J, Dzekov C, Mazer NA, Coviello AD, Knapp PE, Hally K, Pinjic E, Yan M, Storer TW, Bhasin S. Effects of Testosterone Administration for 3 Years on Subclinical Atherosclerosis Progression in Older Men With Low or Low-Normal Testosterone Levels: A Randomized Clinical Trial. JAMA 2015; 314:570-581
- Budoff MJ, Ellenberg SS, Lewis CE, Mohler ER, 3rd, Wenger NK, Bhasin S, Barrett-Connor E, Swerdloff RS, Stephens-Shields A, Cauley JA, Crandall JP, Cunningham GR, Ensrud KE, Gill TM, Matsumoto AM, Molitch ME, Nakanishi R, Nezarat N, Matsumoto S, Hou X, Basaria S, Diem SJ, Wang C, Cifelli D, Snyder PJ. Testosterone Treatment and Coronary Artery Plaque Volume in Older Men With Low Testosterone. JAMA2017; 317:708-716
- Xu L, Freeman G, Cowling BJ, Schooling CM. Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med 2013; 11:108
- Borst SE, Shuster JJ, Zou B, Ye F, Jia H, Wokhlu A, Yarrow JF. Cardiovascular risks and elevation of serum DHT vary by route of testosterone administration: a systematic review and meta-analysis. BMC Med 2014; 12:211
- Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover JL, Bhasin S. Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci 2005; 60:1451-1457
- Corona G, Maseroli E, Rastrelli G, Isidori AM, Sforza A, Mannucci E, Maggi M. Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf 2014; 13:1327-1351
- Ruige JB, Ouwens DM, Kaufman JM. Beneficial and adverse effects of testosterone on the cardiovascular system in men. J Clin Endocrinol Metab 2013; 98:4300-4310
- Elliott J, Kelly SE, Millar AC, Peterson J, Chen L, Johnston A, Kotb A, Skidmore B, Bai Z, Mamdani M, Wells GA. Testosterone therapy in hypogonadal men: a systematic review and network meta-analysis. BMJ Open2017; 7:e015284
- Alexander GC, Iyer G, Lucas E, Lin D, Singh S. Cardiovascular Risks of Exogenous Testosterone Use Among Men: A Systematic Review and Meta-Analysis. Am J Med 2017; 130:293-305
- Hudson J, Cruickshank M, Quinton R, Aucott L, Aceves-Martins M, Gillies K, Bhasin S, Snyder PJ, Ellenberg SS, Grossmann M, Travison TG, Gianatti EJ, van der Schouw YT, Emmelot-Vonk MH, Giltay EJ, Hackett G, Ramachandran S, Svartberg J, Hildreth KL, Groti Antonic K, Brock GB, Tenover JL, Tan HM, Kong CHC, Tan WS, Marks LS, Ross RJ, Schwartz RS, Manson P, Roberts S, Andersen MS, Magnussen LV, Hernandez R, Oliver N, Wu F, Dhillo WS, Bhattacharya S, Brazzelli M, Jayasena CN. Adverse cardiovascular events and mortality in men during testosterone treatment: an individual patient and aggregate data meta-analysis. Lancet Healthy Longev 2022; 3:e381-e393
- Marriott RJ, Harse J, Murray K, Yeap BB. Systematic review and meta-analyses on associations of endogenous testosterone concentration with health outcomes in community-dwelling men. BMJ Open 2021; 11:e048013
- Bhasin S, Lincoff AM, Basaria S, Bauer DC, Boden WE, Cunningham GR, Davey D, Dubcenco E, Fukumoto S, Garcia M, Granger CB, Kalahasti V, Khera M, Miller MG, Mitchell LM, O'Leary MP, Pencina KM, Snyder PJ, Thompson IM, Jr., Travison TG, Wolski K, Nissen SE, Investigators TS. Effects of long-term testosterone treatment on cardiovascular outcomes in men with hypogonadism: Rationale and design of the TRAVERSE study. Am Heart J 2022; 245:41-50
- Bittner V. Lipoprotein abnormalities related to women's health. Am J Cardiol 2002; 90:77i-84i
- Phan BA, Toth PP. Dyslipidemia in women: etiology and management. Int J Womens Health 2014; 6:185-194
- Wang X, Magkos F, Mittendorfer B. Sex differences in lipid and lipoprotein metabolism: it's not just about sex hormones. J Clin Endocrinol Metab 2011; 96:885-893
- Cifkova R, Krajcoviechova A. Dyslipidemia and cardiovascular disease in women. Curr Cardiol Rep 2015; 17:609
- Jenner JL, Ordovas JM, Lamon-Fava S, Schaefer MM, Wilson PW, Castelli WP, Schaefer EJ. Effects of age, sex, and menopausal status on plasma lipoprotein(a) levels. The Framingham Offspring Study. Circulation1993; 87:1135-1141
- Lip GY, Blann AD, Jones AF, Beevers DG. Effects of hormone-replacement therapy on hemostatic factors, lipid factors, and endothelial function in women undergoing surgical menopause: implications for prevention of atherosclerosis. Am Heart J 1997; 134:764-771
- Godsland IF. Effects of postmenopausal hormone replacement therapy on lipid, lipoprotein, and apolipoprotein (a) concentrations: analysis of studies published from 1974-2000. Fertil Steril 2001; 75:898-915
- Lobo RA. Clinical review 27: Effects of hormonal replacement on lipids and lipoproteins in postmenopausal women. J Clin Endocrinol Metab 1991; 73:925-930
- Chait A, Subramanian S, Brunzell JD. Genetic Disorders of Triglyceride Metabolism. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M, Rebar R, Singer F, Vinik A, Weickert MO, eds. Endotext. South Dartmouth (MA)2000.
- Goodman MP. Are all estrogens created equal? A review of oral vs. transdermal therapy. J Womens Health (Larchmt) 2012; 21:161-169
- Smith GI, Reeds DN, Okunade AL, Patterson BW, Mittendorfer B. Systemic delivery of estradiol, but not testosterone or progesterone, alters very low density lipoprotein-triglyceride kinetics in postmenopausal women. J Clin Endocrinol Metab 2014; 99:E1306-1310
- Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA 1995; 273:199-208
- Darling GM, Johns JA, McCloud PI, Davis SR. Estrogen and progestin compared with simvastatin for hypercholesterolemia in postmenopausal women. N Engl J Med 1997; 337:595-601
- Tsuda M, Sanada M, Nakagawa H, Kodama I, Sakashita T, Ohama K. Phenotype of apolipoprotein E influences the lipid metabolic response of postmenopausal women to hormone replacement therapy. Maturitas2001; 38:297-304
- Herrington DM, Howard TD, Hawkins GA, Reboussin DM, Xu J, Zheng SL, Brosnihan KB, Meyers DA, Bleecker ER. Estrogen-receptor polymorphisms and effects of estrogen replacement on high-density lipoprotein cholesterol in women with coronary disease. N Engl J Med 2002; 346:967-974
- Liebeskind A, Thompson J, Wilson D. Reproductive Health and its Impact on Lipid Management in Adolescent and Young Adult Females. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrere B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, eds. Endotext. South Dartmouth (MA)2022.
- Kim JJ, Choi YM. Dyslipidemia in women with polycystic ovary syndrome. Obstet Gynecol Sci 2013; 56:137-142
- Wild RA. Dyslipidemia in PCOS. Steroids 2012; 77:295-299
- Wild RA, Rizzo M, Clifton S, Carmina E. Lipid levels in polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril 2011; 95:1073-1079 e1071-1011
- Wang M, Zhao D, Xu L, Guo W, Nie L, Lei Y, Long Y, Liu M, Wang Y, Zhang X, Zhang L, Li H, Zhang J, Yuan D, Yue L. Role of PCSK9 in lipid metabolic disorders and ovarian dysfunction in polycystic ovary syndrome. Metabolism 2019; 94:47-58
- Vatannejad A, Salimi F, Moradi N, Fouani FZ, Zandieh Z, Ansaripour S, Sadeghi A, Fadaei R. Evaluation of angiopoietin-like protein 3 (ANGPTL3) levels in polycystic ovary syndrome. Life Sci 2020; 263:118595
- Brinton EA. Oral estrogen replacement therapy in postmenopausal women selectively raises levels and production rates of lipoprotein A-I and lowers hepatic lipase activity without lowering the fractional catabolic rate. Arterioscler Thromb Vasc Biol 1996; 16:431-440
- Hargrove GM, Junco A, Wong NC. Hormonal regulation of apolipoprotein AI. J Mol Endocrinol 1999; 22:103-111
- Lamon-Fava S, Postfai B, Diffenderfer M, DeLuca C, O'Connor J, Jr., Welty FK, Dolnikowski GG, Barrett PH, Schaefer EJ. Role of the estrogen and progestin in hormonal replacement therapy on apolipoprotein A-I kinetics in postmenopausal women. Arterioscler Thromb Vasc Biol 2006; 26:385-391
- Schaefer EJ, Foster DM, Zech LA, Lindgren FT, Brewer HB, Jr., Levy RI. The effects of estrogen administration on plasma lipoprotein metabolism in premenopausal females. J Clin Endocrinol Metab 1983; 57:262-267
- Walsh BW, Li H, Sacks FM. Effects of postmenopausal hormone replacement with oral and transdermal estrogen on high density lipoprotein metabolism. J Lipid Res 1994; 35:2083-2093
- Applebaum DM, Goldberg AP, Pykalisto OJ, Brunzell JD, Hazzard WR. Effect of estrogen on post-heparin lipolytic activity. Selective decline in hepatic triglyceride lipase. J Clin Invest 1977; 59:601-608
- Applebaum-Bowden D, McLean P, Steinmetz A, Fontana D, Matthys C, Warnick GR, Cheung M, Albers JJ, Hazzard WR. Lipoprotein, apolipoprotein, and lipolytic enzyme changes following estrogen administration in postmenopausal women. J Lipid Res 1989; 30:1895-1906
- Tikkanen MJ, Nikkila EA, Kuusi T, Sipinen SU. High density lipoprotein-2 and hepatic lipase: reciprocal changes produced by estrogen and norgestrel. J Clin Endocrinol Metab 1982; 54:1113-1117
- Lopez D, McLean MP. Estrogen regulation of the scavenger receptor class B gene: Anti-atherogenic or steroidogenic, is there a priority? Mol Cell Endocrinol 2006; 247:22-33
- Campos H, Walsh BW, Judge H, Sacks FM. Effect of estrogen on very low density lipoprotein and low density lipoprotein subclass metabolism in postmenopausal women. J Clin Endocrinol Metab 1997; 82:3955-3963
- Eriksson M, Berglund L, Rudling M, Henriksson P, Angelin B. Effects of estrogen on low density lipoprotein metabolism in males. Short-term and long-term studies during hormonal treatment of prostatic carcinoma. J Clin Invest 1989; 84:802-810
- Karjalainen A, Heikkinen J, Savolainen MJ, Backstrom AC, Kesaniemi YA. Mechanisms regulating LDL metabolism in subjects on peroral and transdermal estrogen replacement therapy. Arterioscler Thromb Vasc Biol 2000; 20:1101-1106
- Walsh BW, Schiff I, Rosner B, Greenberg L, Ravnikar V, Sacks FM. Effects of postmenopausal estrogen replacement on the concentrations and metabolism of plasma lipoproteins. N Engl J Med 1991; 325:1196-1204
- Parini P, Angelin B, Rudling M. Importance of estrogen receptors in hepatic LDL receptor regulation. Arterioscler Thromb Vasc Biol 1997; 17:1800-1805
- Semenkovich CF, Ostlund RE, Jr. Estrogens induce low-density lipoprotein receptor activity and decrease intracellular cholesterol in human hepatoma cell line Hep G2. Biochemistry 1987; 26:4987-4992
- Windler EE, Kovanen PT, Chao YS, Brown MS, Havel RJ, Goldstein JL. The estradiol-stimulated lipoprotein receptor of rat liver. A binding site that membrane mediates the uptake of rat lipoproteins containing apoproteins B and E. J Biol Chem 1980; 255:10464-10471
- Kovanen PT, Brown MS, Goldstein JL. Increased binding of low density lipoprotein to liver membranes from rats treated with 17 alpha-ethinyl estradiol. J Biol Chem 1979; 254:11367-11373
- Persson L, Henriksson P, Westerlund E, Hovatta O, Angelin B, Rudling M. Endogenous estrogens lower plasma PCSK9 and LDL cholesterol but not Lp(a) or bile acid synthesis in women. Arterioscler Thromb Vasc Biol 2012; 32:810-814
- Persson L, Galman C, Angelin B, Rudling M. Importance of proprotein convertase subtilisin/kexin type 9 in the hormonal and dietary regulation of rat liver low-density lipoprotein receptors. Endocrinology 2009; 150:1140-1146
- Ghosh M, Galman C, Rudling M, Angelin B. Influence of physiological changes in endogenous estrogen on circulating PCSK9 and LDL cholesterol. J Lipid Res 2015; 56:463-469
- Glueck CJ, Fallat RW, Scheel D. Effects of estrogenic compounds on triglyceride kinetics. Metabolism 1975; 24:537-545
- Kissebah AH, Harrigan P, Wynn V. Mechanism of hypertriglyceridaemia associated with contraceptive steroids. Horm Metab Res 1973; 5:184-190
- Tikkanen MJ, Kuusi T, Nikkila EA, Sane T. Very low density lipoprotein triglyceride kinetics during hepatic lipase suppression by estrogen. Studies on the physiological role of hepatic endothelial lipase. FEBS Lett1985; 181:160-164
- Sitruk-Ware R, Nath A. Characteristics and metabolic effects of estrogen and progestins contained in oral contraceptive pills. Best Pract Res Clin Endocrinol Metab 2013; 27:13-24
- Johansson S, Vedin A, Wilhelmsson C. Myocardial infarction in women. Epidemiol Rev 1983; 5:67-95
- Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J 1986; 111:383-390
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, Investigators IS. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:937-952
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric 2015; 18:483-491
- Gordon T, Kannel WB, Hjortland MC, McNamara PM. Menopause and coronary heart disease. The Framingham Study. Ann Intern Med 1978; 89:157-161
- Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med 1976; 85:447-452
- Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause 2006; 13:265-279
- Zhu D, Chung HF, Dobson AJ, Pandeya N, Giles GG, Bruinsma F, Brunner EJ, Kuh D, Hardy R, Avis NE, Gold EB, Derby CA, Matthews KA, Cade JE, Greenwood DC, Demakakos P, Brown DE, Sievert LL, Anderson D, Hayashi K, Lee JS, Mizunuma H, Tillin T, Simonsen MK, Adami HO, Weiderpass E, Mishra GD. Age at natural menopause and risk of incident cardiovascular disease: a pooled analysis of individual patient data. Lancet Public Health 2019; 4:e553-e564
- Lubiszewska B, Kruk M, Broda G, Ksiezycka E, Piotrowski W, Kurjata P, Zielinski T, Ploski R. The impact of early menopause on risk of coronary artery disease (PREmature Coronary Artery Disease In Women--PRECADIW case-control study). Eur J Prev Cardiol 2012; 19:95-101
- Muka T, Oliver-Williams C, Kunutsor S, Laven JS, Fauser BC, Chowdhury R, Kavousi M, Franco OH. Association of Age at Onset of Menopause and Time Since Onset of Menopause With Cardiovascular Outcomes, Intermediate Vascular Traits, and All-Cause Mortality: A Systematic Review and Meta-analysis. JAMA Cardiol 2016; 1:767-776
- Wellons M, Ouyang P, Schreiner PJ, Herrington DM, Vaidya D. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause 2012; 19:1081-1087
- Barrett-Connor E, Bush TL. Estrogen and coronary heart disease in women. JAMA 1991; 265:1861-1867
- Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 2000; 133:933-941
- Grodstein F, Stampfer MJ, Manson JE, Colditz GA, Willett WC, Rosner B, Speizer FE, Hennekens CH. Postmenopausal estrogen and progestin use and the risk of cardiovascular disease. N Engl J Med 1996; 335:453-461
- Henderson BE, Paganini-Hill A, Ross RK. Decreased mortality in users of estrogen replacement therapy. Arch Intern Med 1991; 151:75-78
- Psaty BM, Heckbert SR, Atkins D, Lemaitre R, Koepsell TD, Wahl PW, Siscovick DS, Wagner EH. The risk of myocardial infarction associated with the combined use of estrogens and progestins in postmenopausal women. Arch Intern Med 1994; 154:1333-1339
- Sidney S, Petitti DB, Quesenberry CP, Jr. Myocardial infarction and the use of estrogen and estrogen-progestogen in postmenopausal women. Ann Intern Med 1997; 127:501-508
- Stampfer MJ, Colditz GA, Willett WC, Manson JE, Rosner B, Speizer FE, Hennekens CH. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses' health study. N Engl J Med1991; 325:756-762
- Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, Vittinghoff E. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605-613
- Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, Hsia J, Hulley S, Herd A, Khan S, Newby LK, Waters D, Vittinghoff E, Wenger N, Group HR. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA 2002; 288:49-57
- Shlipak MG, Simon JA, Vittinghoff E, Lin F, Barrett-Connor E, Knopp RH, Levy RI, Hulley SB. Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA2000; 283:1845-1852
- Manson JE, Hsia J, Johnson KC, Rossouw JE, Assaf AR, Lasser NL, Trevisan M, Black HR, Heckbert SR, Detrano R, Strickland OL, Wong ND, Crouse JR, Stein E, Cushman M, Women's Health Initiative I. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003; 349:523-534
- Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, O'Sullivan MJ, Phillips L, Prentice RL, Ritenbaugh C, Robbins J, Rossouw JE, Sarto G, Stefanick ML, Van Horn L, Wactawski-Wende J, Wallace R, Wassertheil-Smoller S, Women's Health Initiative Steering C. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA 2004; 291:1701-1712
- Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, Anderson G, Howard BV, Thomson CA, LaCroix AZ, Wactawski-Wende J, Jackson RD, Limacher M, Margolis KL, Wassertheil-Smoller S, Beresford SA, Cauley JA, Eaton CB, Gass M, Hsia J, Johnson KC, Kooperberg C, Kuller LH, Lewis CE, Liu S, Martin LW, Ockene JK, O'Sullivan MJ, Powell LH, Simon MS, Van Horn L, Vitolins MZ, Wallace RB. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials. JAMA 2013; 310:1353-1368
- Harman SM, Vittinghoff E, Brinton EA, Budoff MJ, Cedars MI, Lobo RA, Merriam GR, Miller VM, Naftolin F, Pal L, Santoro N, Taylor HS, Black DM. Timing and duration of menopausal hormone treatment may affect cardiovascular outcomes. Am J Med 2011; 124:199-205
- Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, Ko M, LaCroix AZ, Margolis KL, Stefanick ML. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA 2007; 297:1465-1477
- Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: Coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med 2006; 21:363-366
- Boardman HM, Hartley L, Eisinga A, Main C, Roque i Figuls M, Bonfill Cosp X, Gabriel Sanchez R, Knight B. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst Rev 2015:CD002229
- Schierbeck LL, Rejnmark L, Tofteng CL, Stilgren L, Eiken P, Mosekilde L, Kober L, Jensen JE. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ 2012; 345:e6409
- Bassuk SS, Manson JE. The timing hypothesis: Do coronary risks of menopausal hormone therapy vary by age or time since menopause onset? Metabolism 2016; 65:794-803
- Bray PF, Larson JC, Lacroix AZ, Manson J, Limacher MC, Rossouw JE, Lasser NL, Lawson WE, Stefanick ML, Langer RD, Margolis KL, Women's Health Initiative I. Usefulness of baseline lipids and C-reactive protein in women receiving menopausal hormone therapy as predictors of treatment-related coronary events. Am J Cardiol 2008; 101:1599-1605
- Wild RA, Wu C, Curb JD, Martin LW, Phillips L, Stefanick M, Trevisan M, Manson JE. Coronary heart disease events in the Women's Health Initiative hormone trials: effect modification by metabolic syndrome: a nested case-control study within the Women's Health Initiative randomized clinical trials. Menopause 2013; 20:254-260
- Wild RA, Hovey KM, Andrews C, Robinson JG, Kaunitz AM, Manson JE, Crandall CJ, Paragallo R, Shufelt C, Merz CNB. Cardiovascular disease (CVD) risk scores, age, or years since menopause to predict cardiovascular disease in the Women's Health Initiative. Menopause 2021; 28:610-618
- Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: does the increased risk ever disappear? A randomized trial. Ann Intern Med 2010; 152:211-217
- Hernan MA, Alonso A, Logan R, Grodstein F, Michels KB, Willett WC, Manson JE, Robins JM. Observational studies analyzed like randomized experiments: an application to postmenopausal hormone therapy and coronary heart disease. Epidemiology 2008; 19:766-779
- Herrington DM, Reboussin DM, Brosnihan KB, Sharp PC, Shumaker SA, Snyder TE, Furberg CD, Kowalchuk GJ, Stuckey TD, Rogers WJ, Givens DH, Waters D. Effects of estrogen replacement on the progression of coronary-artery atherosclerosis. N Engl J Med 2000; 343:522-529
- Hodis HN, Mack WJ, Azen SP, Lobo RA, Shoupe D, Mahrer PR, Faxon DP, Cashin-Hemphill L, Sanmarco ME, French WJ, Shook TL, Gaarder TD, Mehra AO, Rabbani R, Sevanian A, Shil AB, Torres M, Vogelbach KH, Selzer RH, Women's Estrogen-Progestin Lipid-Lowering Hormone Atherosclerosis Regression Trial Research G. Hormone therapy and the progression of coronary-artery atherosclerosis in postmenopausal women. N Engl J Med 2003; 349:535-545
- Waters DD, Alderman EL, Hsia J, Howard BV, Cobb FR, Rogers WJ, Ouyang P, Thompson P, Tardif JC, Higginson L, Bittner V, Steffes M, Gordon DJ, Proschan M, Younes N, Verter JI. Effects of hormone replacement therapy and antioxidant vitamin supplements on coronary atherosclerosis in postmenopausal women: a randomized controlled trial. JAMA 2002; 288:2432-2440
- Angerer P, Stork S, Kothny W, Schmitt P, von Schacky C. Effect of oral postmenopausal hormone replacement on progression of atherosclerosis : a randomized, controlled trial. Arterioscler Thromb Vasc Biol 2001; 21:262-268
- Manson JE, Allison MA, Rossouw JE, Carr JJ, Langer RD, Hsia J, Kuller LH, Cochrane BB, Hunt JR, Ludlam SE, Pettinger MB, Gass M, Margolis KL, Nathan L, Ockene JK, Prentice RL, Robbins J, Stefanick ML, Whi, Investigators W-C. Estrogen therapy and coronary-artery calcification. N Engl J Med 2007; 356:2591-2602
- Hodis HN, Mack WJ, Lobo RA, Shoupe D, Sevanian A, Mahrer PR, Selzer RH, Liu Cr CR, Liu Ch CH, Azen SP, Estrogen in the Prevention of Atherosclerosis Trial Research G. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939-953
- Hodis HN, Mack WJ, Henderson VW, Shoupe D, Budoff MJ, Hwang-Levine J, Li Y, Feng M, Dustin L, Kono N, Stanczyk FZ, Selzer RH, Azen SP, Group ER. Vascular Effects of Early versus Late Postmenopausal Treatment with Estradiol. N Engl J Med 2016; 374:1221-1231
- Roach RE, Helmerhorst FM, Lijfering WM, Stijnen T, Algra A, Dekkers OM. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev 2015:CD011054
- Chakhtoura Z, Canonico M, Gompel A, Scarabin PY, Plu-Bureau G. Progestogen-only contraceptives and the risk of acute myocardial infarction: a meta-analysis. J Clin Endocrinol Metab 2011; 96:1169-1174
- Peragallo Urrutia R, Coeytaux RR, McBroom AJ, Gierisch JM, Havrilesky LJ, Moorman PG, Lowery WJ, Dinan M, Hasselblad V, Sanders GD, Myers ER. Risk of acute thromboembolic events with oral contraceptive use: a systematic review and meta-analysis. Obstet Gynecol 2013; 122:380-389
- Baillargeon JP, McClish DK, Essah PA, Nestler JE. Association between the current use of low-dose oral contraceptives and cardiovascular arterial disease: a meta-analysis. J Clin Endocrinol Metab 2005; 90:3863-3870
- Khader YS, Rice J, John L, Abueita O. Oral contraceptives use and the risk of myocardial infarction: a meta-analysis. Contraception 2003; 68:11-17
- Zhao L, Zhu Z, Lou H, Zhu G, Huang W, Zhang S, Liu F. Polycystic ovary syndrome (PCOS) and the risk of coronary heart disease (CHD): a meta-analysis. Oncotarget 2016;
- de Groot PC, Dekkers OM, Romijn JA, Dieben SW, Helmerhorst FM. PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update 2011; 17:495-500
- Iftikhar S, Collazo-Clavell ML, Roger VL, St Sauver J, Brown RD, Jr., Cha S, Rhodes DJ. Risk of cardiovascular events in patients with polycystic ovary syndrome. Neth J Med 2012; 70:74-80
- Jacewicz-Swiecka M, Kowalska I. Polycystic ovary syndrome and the risk of cardiometabolic complications in longitudinal studies. Diabetes Metab Res Rev 2018; 34:e3054
- Guan C, Zahid S, Minhas AS, Ouyang P, Vaught A, Baker VL, Michos ED. Polycystic ovary syndrome: a "risk-enhancing" factor for cardiovascular disease. Fertil Steril 2022; 117:924-935
- Carmina E, Lobo RA. Is There Really Increased Cardiovascular Morbidity in Women with Polycystic Ovary Syndrome? J Womens Health (Larchmt) 2018; 27:1385-1388
- Meyer ML, Malek AM, Wild RA, Korytkowski MT, Talbott EO. Carotid artery intima-media thickness in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update 2012; 18:112-126
- Gomez JMD, VanHise K, Stachenfeld N, Chan JL, Merz NB, Shufelt C. Subclinical cardiovascular disease and polycystic ovary syndrome. Fertil Steril 2022; 117:912-923
- Talbott EO, Zborowski JV, Rager JR, Boudreaux MY, Edmundowicz DA, Guzick DS. Evidence for an association between metabolic cardiovascular syndrome and coronary and aortic calcification among women with polycystic ovary syndrome. J Clin Endocrinol Metab 2004; 89:5454-5461
- Talbott EO, Zborowski J, Rager J, Stragand JR. Is there an independent effect of polycystic ovary syndrome (PCOS) and menopause on the prevalence of subclinical atherosclerosis in middle aged women? Vasc Health Risk Manag 2008; 4:453-462
- Shroff R, Kerchner A, Maifeld M, Van Beek EJ, Jagasia D, Dokras A. Young obese women with polycystic ovary syndrome have evidence of early coronary atherosclerosis. J Clin Endocrinol Metab 2007; 92:4609-4614
- Chang AY, Ayers C, Minhajuddin A, Jain T, Nurenberg P, de Lemos JA, Wild RA, Auchus RJ. Polycystic ovarian syndrome and subclinical atherosclerosis among women of reproductive age in the Dallas heart study. Clin Endocrinol (Oxf) 2011; 74:89-96
- Christian RC, Dumesic DA, Behrenbeck T, Oberg AL, Sheedy PF, 2nd, Fitzpatrick LA. Prevalence and predictors of coronary artery calcification in women with polycystic ovary syndrome. J Clin Endocrinol Metab2003; 88:2562-2568